Blog
We are constantly learning so that, with wisdom and good stewardship, we can utilize the best research-backed techniques, materials, and treatments. We believe that excellence matters in all aspects of our care, and it shows.
Tongue and Lip Ties Part 2: Gathering Information and Consultations
We read books, researched online, listened to podcasts, and had consultations with 5 professional healthcare providers before making our decision about our son’s lip and tongue tie. Here’s what we learned!
As parents our emotional journey leading up to my son's release procedure was a rollercoaster of anxiety, uncertainty, and determination. We were somewhat anxious through the entire process but our unwavering commitment to our son's well-being ultimately led to the decision to proceed with getting his ties released. Along the way, we researched on our own and consulted with various healthcare professionals to ensure we would make the best choice for our child. Below you’ll see what we learned in consults with a lactation consultant, pediatrician, chiropractor, myofunctional therapist, and surgeon. Then I’ll describe the procedure itself!
In case you missed it:
Part 1 defines a tongue or lip tie and discusses the associated risks
Part 2, this post, describes our emotional journey as parents, the consultations we had, and ultimately the procedure itself
Part 3 describes what happens after the frenectomy – home care and healing process
Because of my training as a dentist, I knew the risks of leaving a tie untreated (see the first post in this series) and I was familiar with the release procedure having performed it myself. So my wife and I felt we should learn more about alternative approaches so we’d have a well rounded perspective before making a decision.
Outside of professional guidance, some of the resources we used were:
Dr Ghaheri’s blog and website: Excellent all around resource. Dr Ghaheri is an ENT but offers a balanced perspective and respects the role of other providers in treating possible tongue and lip tie
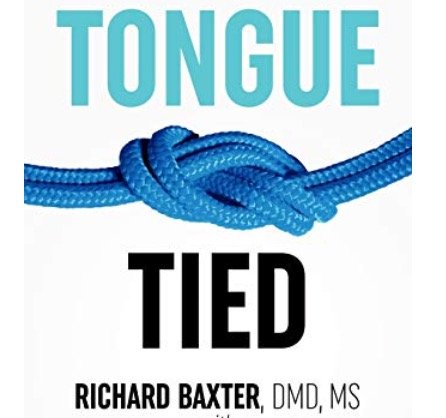
Tongue Tied book by Dr Richard Baxter: Lots of great information from a pediatric dentist and a team of other providers who treat tongue tie routinely.
Freely Rooted podcast: The Big Picture of Tongue Ties: A podcast episode with a conservative perspective on why not every frenum is a “tongue tie”, and emphasizes a holistic approach
The specialists we consulted with were a lactation consultant, a chiropractor, a myofunctional therapist, a pediatrician, and finally the surgeon who ended up doing the release procedure. Below I’ll describe our experience with each.
Lactation Consultant Consult:
This is the first place anyone with questions about breastfeeding issues should start. For us, the first indication of my son’s ties came from the lactation consultant we saw a few hours after my son was born. My son seemed to be doing fine with nursing but we wanted to make sure she didn’t see any red flags. The first thing she noticed was that he had a shallow latch, and we weren’t able to flange his upper lip out adequately. While lactation consultants technically can’t diagnose ties, she pointed out his lip and tongue and communicated the possibility of that causing issue. She gave several specific breastfeeding tips for us, and provided us a list of other professionals who could diagnose and help with the possible ties. Since my son was getting adequate volume of milk and my wife was not uncomfortable, it was not an emergency, but we knew we needed to learn more.
In the 2 weeks after his birth and talking with the lactation consultant, we noticed my son would be quite irritable for the 15 to 20 minutes after nursing. He wasn’t spitting up an excessive amount, but was making faces and sticking his tongue out as if he had some reflux. He also seemed a little more gassy than our first child. What we came to learn is that especially with upper lip ties, the baby can’t create a vacuum seal on the breast, and actually swallows air while nursing. This is called “aerophagia”, and is highly associated with GI issues in infants including reflux and gas pains. Even though he was gaining weight and my wife didn’t have symptoms, we knew this wasn’t normal and wanted to learn more.
A blister is indicative of a poor latch
An indicator of upper lip tie may be a blister on the infant’s lip. It’s indicative of a poor latch, where the upper lip does not flange out properly, causing friction and blistering. Here you can see the blister and tie. Image courtesy of Dr Ghaheri. He’s a great resource.
Pediatrician consult
Our pediatrician also gave us valuable information. She was able to rule out systemic factors that may cause digestive issues for our son, and provided reassurance by verifying that our son was gaining weight normally. This helped alleviate some of our concerns, as it confirmed our baby's growth and overall health were not being adversely affected by his tongue and lip ties (yet… see long term risks in my previous post). Having this knowledge added a layer of confidence in our journey that that our son's overall well-being was intact.
Chiropractor Consult:
When a tongue or lip tie is present, alternative strategies to address it involve making sure the surrounding tissue and fascia are not too tight. Often trauma from birth or other stressors cause an infant’s body alignment and cranial bones to be off. Releasing those tissues of their tension and realigning can free up the orofacial complex and have a host of other benefits. Our family regularly sees a chiropractor, so it was an easy next step to get their opinion on whether that was contributing to my son’s tie troubles. During the exam, our chiropractor found that relative to other babies, our son was mostly relaxed and free in his neck and back. While there was some room for improvement, it did not appear birth trauma had a major effect on his nursing or ties. This was enlightening, but we still wanted to learn more.
Myofunctional Therapist Consult:
Initially, we wanted to have a consult with the surgeon who would possibly do my son’s release, and their office recommended we see a myofunctional therapist first. We went to BDI Playhouse in Aurora, Illinois. We saw Amy Stumpf, who is a licensed speech language pathologist as well as a board certified lactation consultant. We had a great experience! In her exam she was able to reaffirm what the chiropractor told us, and also noted the relative severity of my son’s ties. She gave us some specific exercises to help, but said that while for many children myofunctional therapy alone can solve breastfeeding issues, it would likely be insufficient given the severity of our son’s ties. She was willing to work with us if we didn’t want to get the ties released, her opinion was clear.
After our visit with the therapist, our parental anxiety increased somewhat. A part of us wanted a good reason to avoid the releases if possible. It was just hard to imagine the discomfort our little guy would have during and after the procedure. At this point, we thought we knew the best choice. But we wanted to see what the surgeon had to say first.
Surgeon consult:
The surgeon we saw came highly recommended from my dental colleagues and lactation consultants alike: Dr Milton Geivelis in Elgin, Illinois. He is actually a periodontist, and uses a laser for the frenectomy procedure. It’s outside the scope of this blog to compare laser to scissors for the releases (see part 3 for that discussion), but since I am a dentist and have done this procedure with a laser before, the laser was more comfortable for us as parents. This is generally what I recommend for my patients as well.
In our consult with the surgeon, he recommended releases. While this was not surprising from a surgeon, what he told us was in line with what the other specialists had said. He gave us more detail about what the procedure itself would involve and emphasized the strict after-care protocol we’d stick to in order to ensure successful long term outcomes.
In the end, we knew what we had to do.
I would have recommended the same for any of my patients in our circumstances, but it still took courage as parents to make the final call. We prayed for wisdom and discussed among ourselves. In the end, we scheduled the releases.
By the way… Should you try bottle feeding?
Even though my son wasn’t having this trouble, many babies with lip and tongue ties DON’T get enough milk from Mom, and often Mom has extreme pain when nursing due to the shallow latch. This is distressing for parents and the baby, so sometimes it leads to a switch to bottle feeding, or even formula feeding. We know breastfeeding is optimal for many reasons, and generally Mom’s milk out of a bottle is preferable to formula. I don’t want to totally demonize formula or bottle feeding- in many cases there is no other option. There’s always a risk/benefit analysis to be done. Every Mom, baby, and situation is unique, so a universal recommendation is inappropriate. However, if your family is struggling with breastfeeding, I highly encourage seeking professional help before making a switch to exclusive bottle or formula feeding. At the end of this post are resources to learn more.
The Day of the Frenectomy Procedure:
As a dentist, I knew this procedure would be quick and simple. Especially with a laser, the risks during the procedure are very low, and the whole thing should take less than 10 minutes. Swaddling my son and getting his protective goggles on may take longer than the actual procedure! As a Dad though, I had a mix of emotions. Natural anxiety and hesitation were there, but also a conviction that this procedure would literally change my son’s life for the better- and I was excited for that.
The 10-minutes my son was away from us didn’t actually feel that long. Afterward when we held our son again, a wave of relief washed over us. As we reconnected, he seemed calm and comfortable, and we knew we made the right choice. We were so thankful! Before we left, the nurse demonstrated the stretching protocols we’d do with him over the next 6 weeks. We will talk more about that in our third post in this series.
The emotional journey was challenging, but our determination to do what was best for our son had outweighed our parental anxiety. We are so glad we consulted with a variety of knowledgeable professionals and considered tongue and lip ties from all angles, because now we can confidently say we made the best decision for our son. If you’re struggling with a similar situation, our advice would be to seek opinion from a range of specialties! The best choice for your little one may be different than ours.
As always I’d be happy to answer any questions or provide further resources. Thanks for reading.
Dr Brayden Teuscher
Additional References:
Smith, A. B., & Johnson, C. D. "Tongue and Lip Ties: A Comprehensive Guide for Parents." Journal of Pediatric Health
Taylor, E. L., & Brown, S. M. "Myofunctional Therapy and Its Role in Infant Health." Pediatric Dentistry Today
Walker, L. M., & Davis, J. R. "Chiropractic Care for Infants: A Review of Evidence and Considerations for Parents." Journal of Pediatric Care
Smith, J. R., & Johnson, L. K. "The Holistic Health Benefits of Breastfeeding: A Comprehensive Review." Journal of Pediatric Health and Nutrition
Brown, A., & Harries, V.. "Benefits of Breastfeeding: A Holistic Approach to Infant Health." Pediatric Nursing
Untethering the Secrets of Tongue and Lip Ties: A Three part letter to Moms
I had the medical knowledge. But when my son was diagnosed with a tongue and lip tie, the stakes got higher! Here is mother and father’s journey in navigating his tongue and lip ties.
Dear Moms,
I’m a father of 2 beautiful young boys, aged 2 and now 1 month! Being their Daddy is one of my greatest joys – and most profound responsibilities. Any parent wants the best for their children, but as any new parent realizes – there’s no 5 step parenting manual for perfect parenting! My wife and I are far from perfect parents (who can relate??!) but we are constantly seeking guidance and learning more. The weight of responsibility often feels heaviest with health decisions for our little ones, especially when there’s a level of uncertainty involved.
At our dental practice, we see a ton of kids and I’m constantly talking with parents about the growth of their kids’ jaws and tooth development. I’ve done extensive research on what factors influence this development and how jaw development affects their overall well-being. I felt very comfortable with my perspective on these issues. BUT when my second son was born with a tongue and lip tie, the stakes got higher! I had the knowledge, but still felt a protective father’s anxiety over how to best help my little guy. And my wife and I wanted to learn more.
Our family
As our family navigated this journey, we doubled down on researching tongue and lip ties from all perspectives. Ultimately we decided it was best for our son to get his tongue tie and lip tie released, but along the way we learned a lot and talked with many other parents who were going through the same dilemma. In this three part series I’m going to share the insights we gained, particularly from a holistic perspective, to help empower you to make informed decisions for your own little one.
Part 1 defines a tongue or lip tie and discusses the associated risks
Part 2 describes our emotional journey as parents, the consultations we had, and ultimately the procedure itself
Part 3 describes what happens after the frenectomy – home care and healing process
**Disclaimer – I will not be advocating that every frenum get released. That decision is always made after first considering all the risk factors unique to your own child, from a multidisciplinary perspective. Just because frenectomies were the choice we made does not mean that’s the best route for your own child. I just want to share our experience. I hope it helps you and your family!
Part 1: The Hidden Risks of Untreated Tongue and Lip Ties
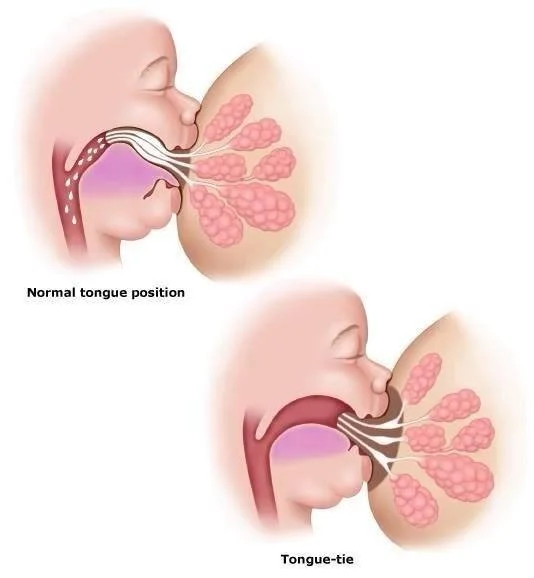
You may have heard the terms "tongue tie" or "lip tie", but what does this actually mean? Simply put, they are congenital conditions where a band of tissue known as the frenulum, or frenum, restricts the movement of the tongue or upper lip. In infants, these ties can affect their ability to breastfeed, causing pain and frustration for both mother and baby. This is how they are most often recognized, so it’s where we will begin:
Breastfeeding issues
For the baby, a tongue or lip tie can limit their ability to latch onto the breast effectively, leading to a shallow latch or painful nursing. This can lead to poor weight gain, frustration, and decreased milk ingestion. Also, infants with ties may experience excessive gas or colic due to swallowing air while feeding. As a result, the baby may not receive adequate nutrition and can become fussy or irritable, affecting their overall growth, development, and, as is often the frustration of new parents: poor sleep.
For the mother, breastfeeding a baby with a tongue or lip tie can be painful and frustrating. The improper latch and inefficient milk transfer can lead to cracked, sore nipples, mastitis, and a decreased milk supply. Mothers may become discouraged and stressed, impacting their overall well-being. Post partum recovery is hard enough without these issues!
Latch Differences
Notice the tongues ability to pull the nipple to the roof of the mouth and latch over the entire areola, versus the shallow latch and lesser milk flow in a tongue tie.
Image from DRGHAHERI.COM, a great resource to learn more.
But wait…
How do you know whether these symptoms are caused by a tongue and lip tie? Often there are actually many factors at play! Birth trauma, tight neck muscles, or fascia issues can also contribute to breastfeeding challenges. That's why seeking the expertise of professionals is so valuable. The first place any mom and baby should go when breastfeeding problems arise is an IBCLC (international board certified lactation consultant) and get their thoughts. An orofacial myologist, physical therapist, chiropractor’s opinion may also be valuable, and we sought all of these in our own journey. (notice- we did not only rely on my training and research as a dentist! A multi-disciplinary perspective is so critical.) These professionals can assess your child's overall orofacial development and help you identify any underlying issues that may be contributing to breastfeeding difficulties. They can also guide you in deciding whether a tongue and lip tie release procedure is necessary for your child.
Here are photos of my son’s ties. There are various ways to grade the severity of these ties- The consensus diagnosis for these would be Class 4 lip tie and Class 3 tongue tie in the other photo.
Other risks involved with tongue and lip ties are less obvious or can show up later in development.
Brain Development
One of the lesser-known but hugely important risks of untreated tongue and lip ties is their potential impact on brain development. The tongue plays a crucial role in the development of the oral and facial muscles, which, in turn influences the development of the cranial bones. If a tongue tie restricts a baby's ability to move their tongue freely, it can lead to altered oral motor patterns. The tongue is directly linked to the brain's sensory and motor regions, making it a critical player in a child's early cognitive development. It plays an indirect role in sleep quality as well.
Sleep Quality
This issue can show up right away in life! As parents, we all know the value of a good night's sleep for both our babies and ourselves. Sleep is crucial for growth and development, and tongue and lip ties can disrupt the harmony of bedtime. Aside from reflux and digestive troubles from poor feeding, tongue ties are highly associated with sleep-disordered breathing patterns in kids and adults. Improper tongue posture can lead to mouth breathing, which is associated with lessened sleep quality. In young children whose brains are developing so rapidly, this can have life-changing consequences. Not only is long term brain development and maturation compromised by poor sleep, but a child’s next-day behavior will be different too. Think of your child when they are tired. They’re probably more irritable, less obedient, more challenging, and despite poor rest are possibly even more energetic than normal. There’s a lot of thought that the poor sleep from mouth breathing has led to an increase in clinical diagnoses like ADHD in kids. I could write a ton more on this topic but am leaving it at that for the sake of (relative) brevity.
The bottom line is that the brain does not grow and develop optimally without proper sleep, and mouth breathing prevents proper sleep.
Respiratory and immune health
As kids grow, the inability to have ideal oral posture will also restrict the tongue’s ability to rest against the palate and naturally push the upper jaw out and forward. Since the upper jaw is the base of the nasal airway, the effect of a baby’s mouth-breathing snowballs into a narrow-palate teenager or adult who is all but forced to be a perpetual mouth breather! (Check out Napolean below!)
Nasal breathing provides a natural filtration system, humidifying and warming air before it reaches the lungs. This natural system is a huge part of our immunity against airborne viruses, bacteria, and other pollutants or allergens. Mouth breathing is also highly associated with sleep apnea in adulthood, which is strongly correlated with a host of other metabolic and psychiatric illnesses.
Attractive Jaw Development
Your child's smile is not just a charming feature but also a reflection of their overall oral and facial development. We’ve seen above that a tongue or lip tie can affect the oral posture of your child, which can lead to a series of esthetic issues. These include misaligned teeth, a narrow palate, and a slack jawed appearance. “Long face syndrome” distinguishes this pattern of growth from a wider, more defined and square jawline. See my friends Napolean and Superman below.
Compare Henry Cavill’s jaw development to Napolean Dynamite. Notice Napoleans longer and more narrow face/jaw structures and open mouth posture. You can note the bags under his eyes and the inattentive gaze. Cavill (Superman!) has a more defined, square jaw. His lips are shut as he nose breathes. Napolean mouth breaths so much he needs some extra chapstick (“But my lips hurt real bad!”)… I wonder if Napolean has a tongue tie!
The impact of these esthetic issues may not be immediately apparent, but they can manifest later in life. By addressing tongue and lip ties early on, you can promote healthy oral development and potentially prevent the need for orthodontic treatment in the future. This potentially saves time, money, and inconvenience for your child later in life during orthodontic treatment, and strongly contributes to a healthy, attractive jawline as an adult.
Speech Development: Untreated tongue and lip ties can impact speech development, because they restrict the movements of the tongue and lips. These conditions may lead to speech articulation problems, making it challenging for children to pronounce certain sounds correctly. The sequelae of restricted communication, reduced confidence, and possibly poorer academic performance “speak” for themselves (pun intended!) Speech language pathologists are a wonderful resource.
Beyond Breastfeeding: Seeking Professional Guidance
In conclusion, it's crucial for discerning parents like you to be aware of the hidden risks of untreated tongue and lip ties. These conditions can affect not only breastfeeding but also brain development, sleep quality, speech, and esthetic jaw development. By consulting with the right professionals you can address the root causes and make informed decisions for the well-being of your little ones.
As my own journey with my son's ties unfolded, we decided we wanted to address the root cause of all these issues, which in his case was the tongue tie and lip tie. But contemplating the frenectomy procedure for our little guy was hard! I’ll talk more about that in the next part of this series and explore the various alternative treatment options.
I’ve got a list of books and resources on this subject if you’d like to learn more! The list below is a good place to start. Please reach out with any questions.
Dr. Brayden Teuscher
References:
Smith R, et al. (2015) "Tongue-tie: the evidence for division and the significance of professional and parental attitudes." International Journal of Pediatric Otorhinolaryngology.
Geddes DT, et al. (2008) "Frenulotomy for breastfeeding infants with ankyloglossia: effect on milk removal and sucking mechanism as imaged by ultrasound." Pediatrics.
Guillemin M, et al. (2013) "Ankyloglossia as a risk factor for maxillary hypoplasia and temporomandibular joint dysfunction." The Angle Orthodontist.
Lowe A, et al. (2012) "Tongue tie and lip tie: evidence and response." Clinical Lactation.
Martinelli RL, et al. (2016) "Ankyloglossia: The adolescent and adult perspective." International Journal of Pediatric Otorhinolaryngology.
https://www.drghaheri.com/blog
BOOKS BELOW
Walker, M. (2017). Why We Sleep: Unlocking the Power of Sleep and Dreams. Scribner.
Moore, S. (2018). Sleep Wrecked Kids: Helping Parents Raise Happy, Healthy Kids, One Sleep at a Time. Grammar Factory
Nestor, J. (2020). Breath: The New Science of a Lost Art. Riverhead Books.
Buchanan, S. (2019). Jaws: The Story of a Hidden Epidemic. Chelsea Green Publishing.
Gelb, M., & Howley, H. (2019). Gasp: Airway Health - The Hidden Path to Wellness. HarperOne.
McKeown, P. (2015). The Oxygen Advantage: The Simple, Scientifically Proven Breathing Techniques for a Healthier, Slimmer, Faster, and Fitter You. William Morrow.
COVID-19 and Tooth Sensitivity
Unwanted Dental Side Effect of Certain Vitamin…During this pandemic we’re all doing our best to stay well. Staying home, “Social Distancing”, washing hands, not touching faces, getting plenty of sleep and fluids, and eating a healthy diet are the…
Having COVID is no fun. Most of us will use our entire arsenal to get better quickly! We’ve all heard that staying home, “Social Distancing”, washing hands, not touching faces, getting plenty of sleep and fluids, and eating a healthy diet are the standard pieces of advice. And did you know the severity of COVID illness is related to gum health? All these things make sense! One recommendation may have an unwanted side effect though.
Vitamins
During the pandemic and when sick with COVID, some of us also choose to take extra vitamins, including Vitamin C. While Vitamin C is generally considered safe for most people to take, the World Health Organization and the Centers for Disease Control and Prevention, and many other sources indicate that there is no clear evidence that Vitamin C is helpful for prevention or cure of COVID-19. However, there are studies indicating Vitamin C deficiency seems to be correlated with people being more susceptible to infections and pneumonia, and also with having a lowered immune response.
So for those who do choose to take Vitamin C as part of their fight against coronavirus, it may be helpful to know that one little-known but common side effect of taking Vitamin C can be Tooth Sensitivity: a brief sharp pain that often happens when a person eats or drinks something very cold or hot.
Tooth Sensitivity
The causes of sensitive teeth can include a cavity, cracked tooth, broken filling, teeth grinding, gum disease, receding gums, or worn enamel. Another cause of this sensitivity can be acid erosion. Acid erosion happens when the enamel of a tooth is exposed to acidic food or drink, stomach acid, or things such as Vitamin C – particularly if it’s the chewable kind. This acidity can cause the enamel to lose minerals and soften. While this softening can be temporary, if the tooth enamel is repeatedly exposed to acid it will gradually erode to leave the underlying dentin exposed and nerves irritated.
What You Can Do
If your tooth sensitivity becomes constant, painful, or you experience swelling or other additional symptoms, call us to discuss before it becomes worse. If your sensitivity remains mild, and you tend to eat or drink acidic things – or you’re taking Vitamin C – there are options you can try to gain some relief and also help prevent additional enamel erosion and future problems:
Reduce your intake of acidic drinks such as sport drinks, fruit juices, etc., and drink them quickly or use a straw to limit the amount of time the liquid lingers on your teeth. Swish your mouth with water afterward.
If you are chewing Vitamin C, consider switching to a different form of C that doesn’t remain in your mouth so long. Also swish with plain water afterward, or even swish water with a little baking soda mixed in it – and then spit it out.
Avoid acidic foods, drinks and vitamins right before bed or while exercising when you produce less cleansing saliva.
Use a soft-bristled toothbrush, and brush more gently.
Switch to a toothpaste made specifically for sensitive teeth.
Avoid tooth-whitening treatments, which often increase sensitivity.
Talk with us. There’s a possibility your pain may be caused by high spots or teeth grinding. This is far more common than you may think, and we may be able to help alleviate your pain with simple remedies.
Dry Mouth and Tooth Sensitivity
A constant flow of saliva is our natural defense against acid erosion and tooth sensitivity. However, some prescription medications as well as over-the-counter medications such as decongestants can cause dry mouth. Incidentally, dry mouth is also a risk factor for other serious concerns including oral cancer (see our post on oral cancer for more information). Staying hydrated with pure water is a good first step. If dry mouth is a continued issue for you, be sure to let us know. There are helpful products that can bring relief to this dryness, and we’ve found that some products are more effective for our patients than others. Keep in mind that mouth dryness can have serious consequences so it’s not something to simply dismiss!
The Bottom Line
We all want to do everything we possibly can to keep our families and ourselves healthy. But sometimes our efforts to be safe in one area of life can cause problems in other areas, as in the case of chewing Vitamin C. It’s tempting to try the many suggested home remedies we hear or read about on the internet, but these ideas can be unhealthy or even dangerous. The wisest thing to do is to stick with respected sources for information, such as the Mayo Clinic, Johns Hopkins, the World Health Organization, the Centers for Disease Control and Prevention, the Teuscher Legacy Health Blog, and, of course, call your physician and/or call us when you need individualized advice and questions answered. We are always happy to help.
Stay healthy!
P.S.- if you have any questions about this, or are in need of cosmetic dentistry, implant dentistry, or general dentistry in St Charles, Illinois, give us a call or text! We’d love to help!
Two Crucial Cold Weather Health Tips to Know Today!
Lots of sane people love winter weather, but I’m not one of them. Give me the hot sun any day. But everything in life gives us an opportunity to learn, and cold weather is no exception. Here are two cold weather essentials you should know: 1. Nose Breathing is best…
Lots of sane people love winter weather, but I’m not one of them. Give me the hot sun any day. But everything in life gives us an opportunity to learn, and cold weather is no exception.
Here are two cold weather essentials you should know:
1. Nose Breathing is best in cold weather – and the rest of the time too.
Studies show that breathing through your nose (as opposed to breathing through your mouth) not only warms the cold winter air, and cleans and humidifies the air – all good for lung health, but nose-breathing may also improve your memory. Memories have 3 main stages of development: encoding, consolidation & retrieval, and according to a recently published Journal of Neuroscience study, nose breathing – but not mouth breathing – enhances all three of these memory stages. For the athlete in all of us, it’s interesting to note that the nasal-pulmonary reflex closes the lungs when the nose closes and opens the lungs when the nose is more open – the Cleveland Clinic says this may be why elite athletes like using nasal strips during exercise. Nose breathing also warms the air before reaching our delicate lungs, humidifies the air for our throat and lungs, and helps clean the air of bacteria, viruses, allergens, pollutants, dust and more before that air reaches your lungs.
2. Pay Attention to the Warning of Cold Sensitivity when it comes to your teeth.
This is no small thing. According to the ADA, causes of sensitive teeth include tooth decay, cracked teeth, worn tooth enamel, worn fillings, and tooth roots that are exposed because of periodontal (gum) disease, gum recession or even from too-aggressive tooth brushing. The Mayo Clinic says that periodontitis, a form of gum disease, can not only cause tooth loss but some research suggests that the bacteria responsible for periodontitis can enter the bloodstream through gum tissue, possibly affecting your heart, lungs, and other parts of the body. Periodontitis may be linked with respiratory disease, rheumatoid arthritis, coronary artery disease or stroke.
If your teeth are sensitive to cold air, it can be vitally important to heed this warning and take action now with your dentist because periodontal disease can be quite serious, and because other causes of cold sensitivity may be way easier to treat when caught early.
So let the cold weather be an opportunity to learn about your health, and a motivation to take positive action! As always, I’d be honored to help you in any way I can.
Your grateful partner in health,
Dr. Mike