Blog
Useful and free info on dental implants, cosmetic dentistry, family dentistry, and more. All posts written by our doctors, not AI or some outside marketing firm. If you are in Campton Hills, St Charles, Geneva, Batavia, Elburn, Elgin, or anywhere in Kane County, these posts will be helpful!
Real Bone Graft Case Part 2: Socket Preservation Graft Healing, CBCT Implant Planning, and Implant Surgery Day
See how we planned this implant case in our 3D software!
Published by Teuscher Legacy Dental – St. Charles, IL
In Part 1, we walked through this patient’s painful failing tooth, gentle extraction, and the placement of a socket preservation bone graft to maintain bone volume for a future dental implant.
In Part 2, we’re going to show you how this graft healed, how we planned and executed implant placement (see the Youtube video for more detail), and what you can expect next as the implant fuses to bone.
1 Week After Socket Preservation — Early Healing
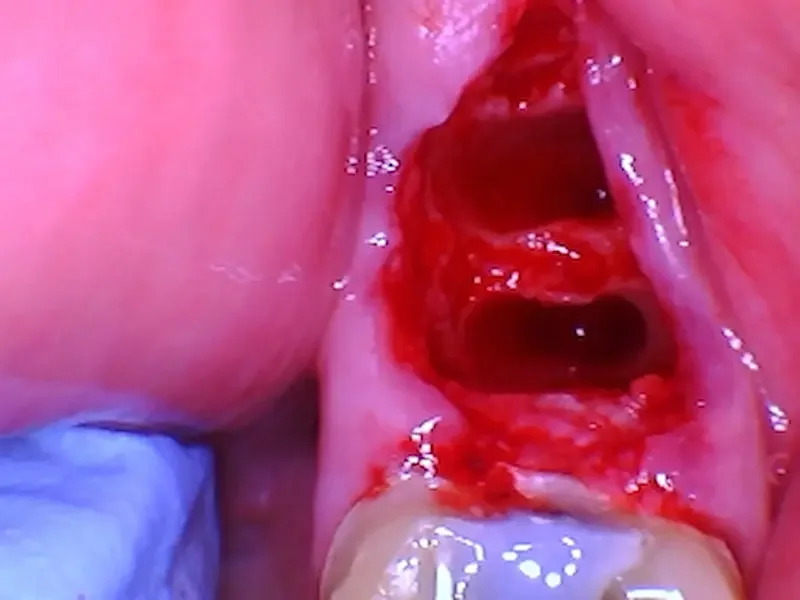
One week after the extraction and bone graft surgery. The tissue is closing nicely, and is pink rather than deep red. Soreness was minimal. The yellow color in the center is normal, immature bone! This site is healing well.
One week after the graft, you can already see how the socket is filling in and the gum tissue is healing nicely. This early phase is all about blood clot stabilization and soft tissue coverage, which protect the graft material while the body begins to lay down new bone. Socket preservation grafts act like a scaffold the body uses to regenerate bone — almost like planting seeds in a garden and letting nature do the rest.
Bonus: Do you really need a bone graft after tooth extraction?
Key things to notice in the photo:
The gum tissue is pink and healthy with minimal swelling, and slowly closing over the extraction socket.
You may see some residual graft particles near the surface — this is normal. There aren’t any in this picture.
There’s no sign of infection, pain, or deep redness — this is an excellent early healing response.
Healing like this tells us the socket preservation graft is doing its job — maintaining ridge height and width so future implant placement will be predictable.
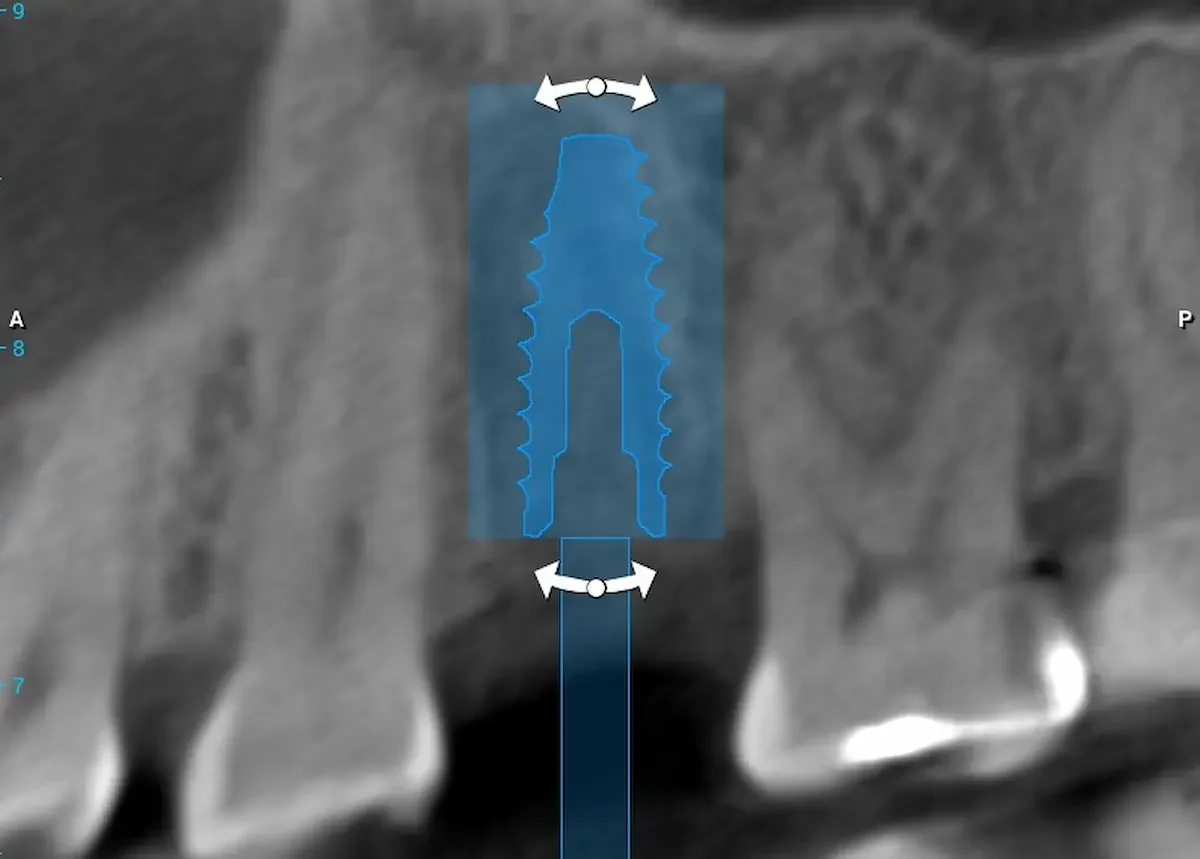
3D Imaging & Implant Planning
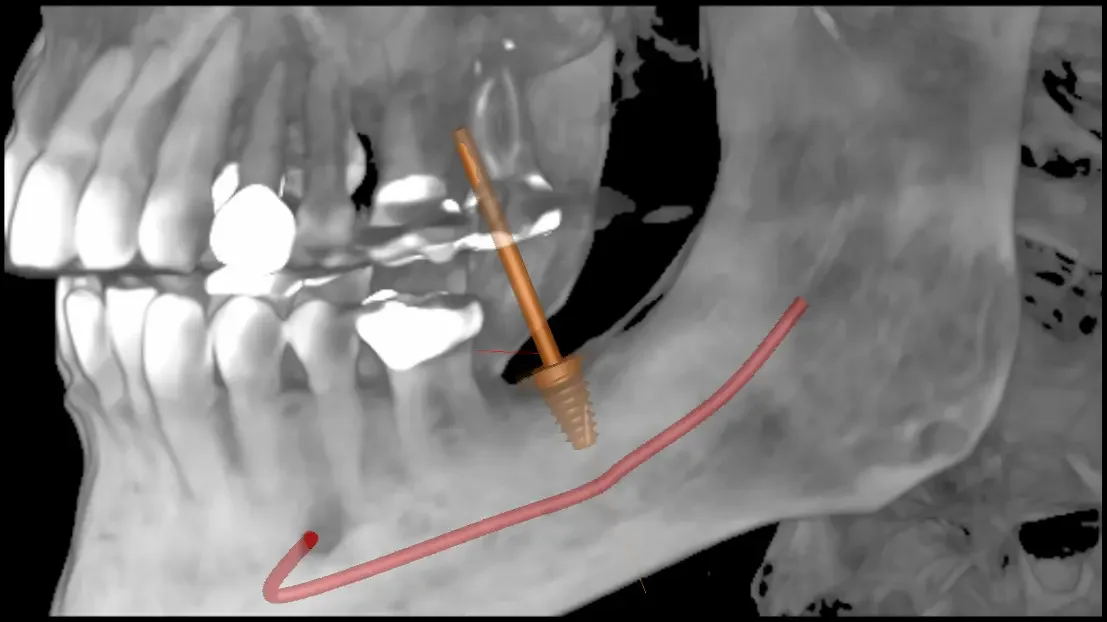
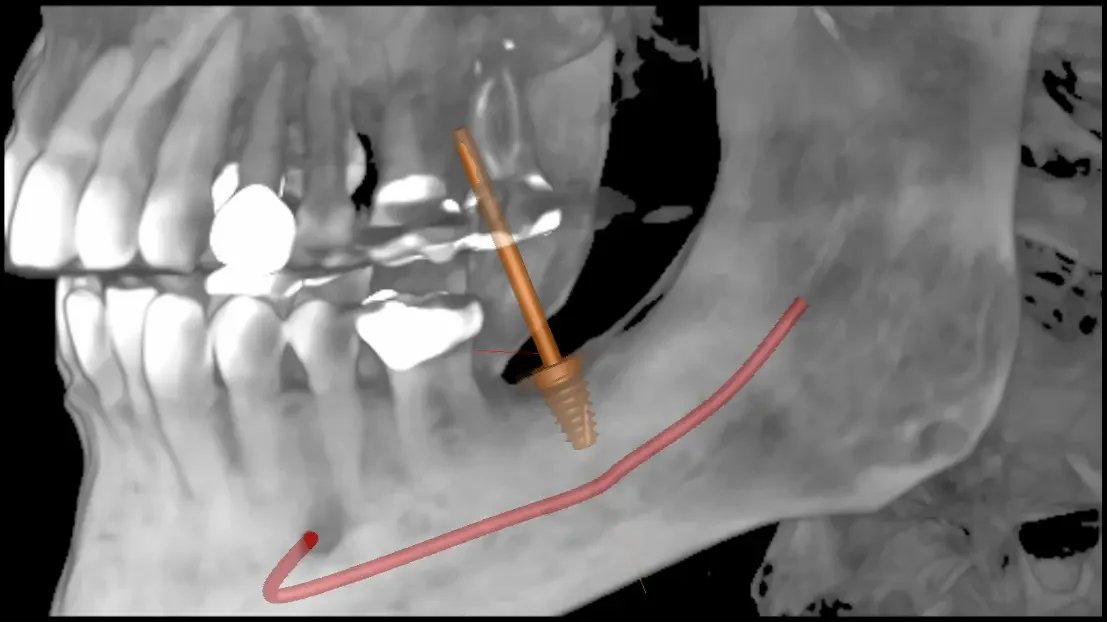
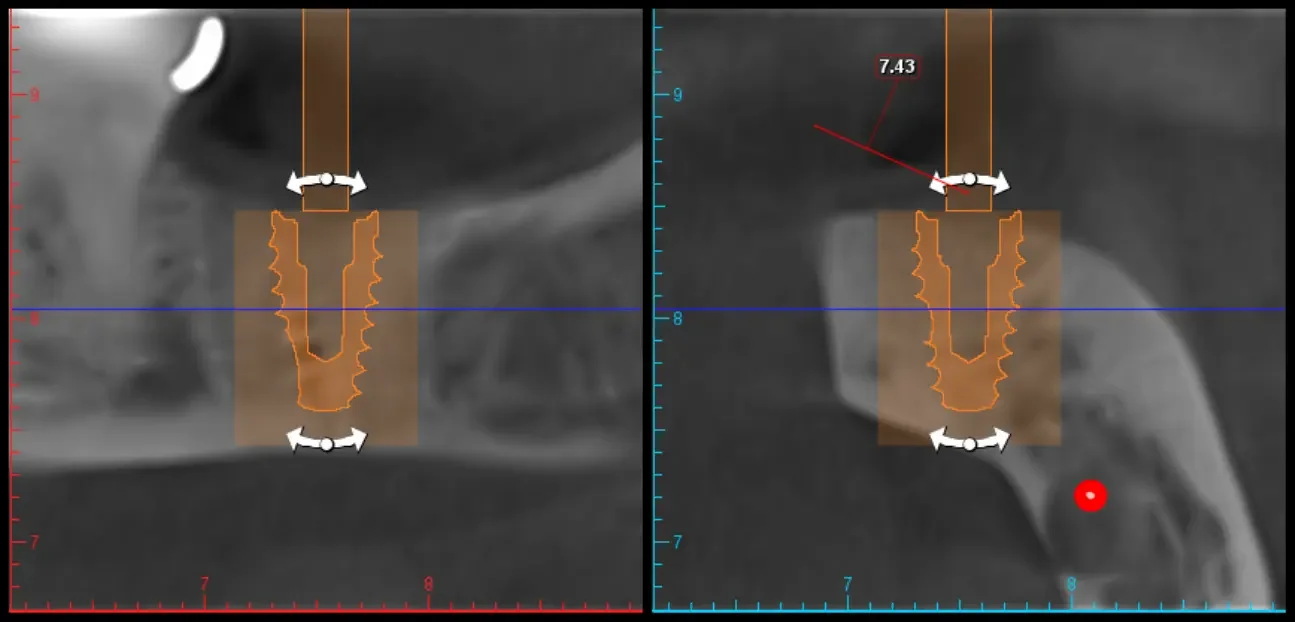
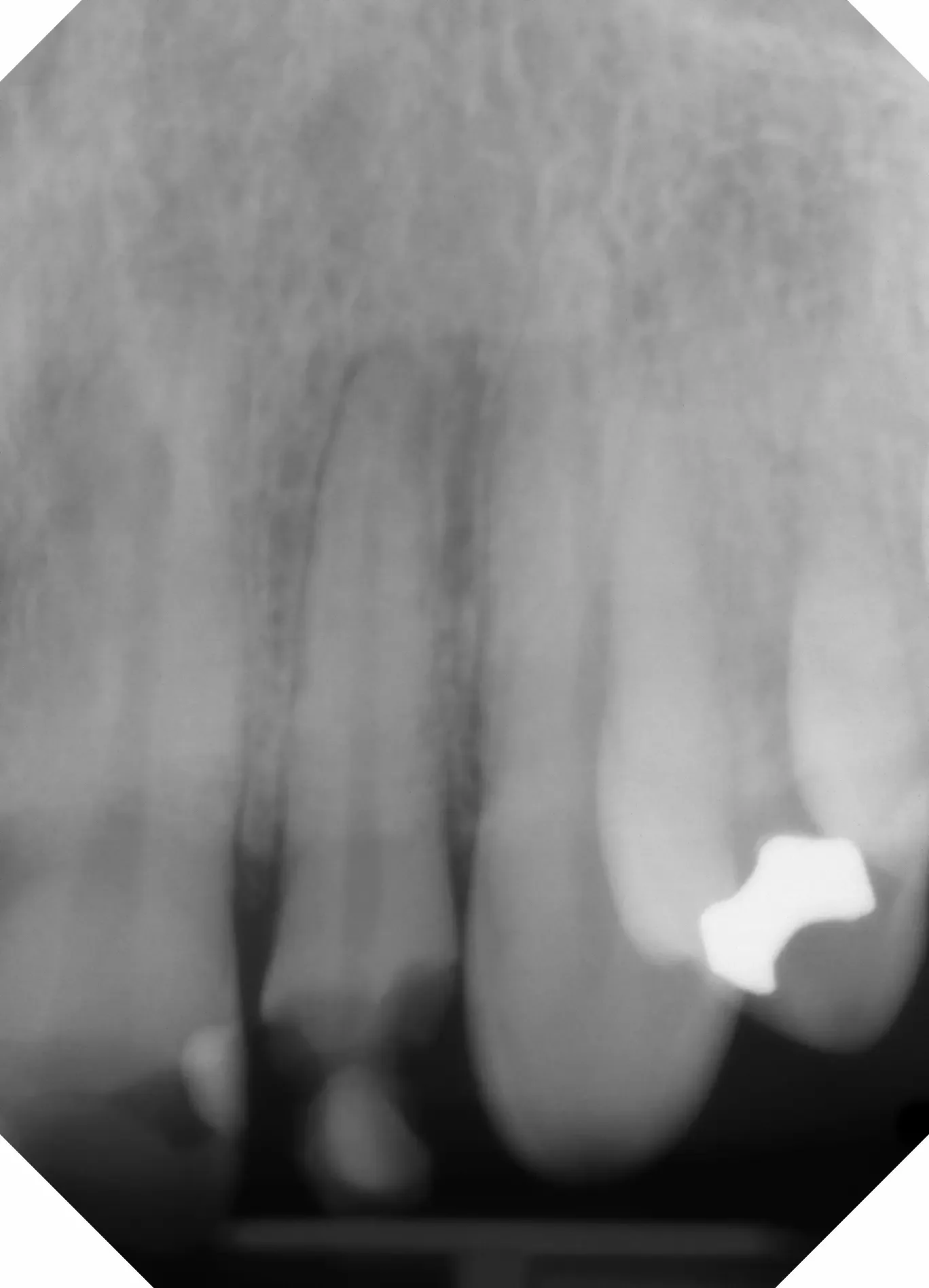
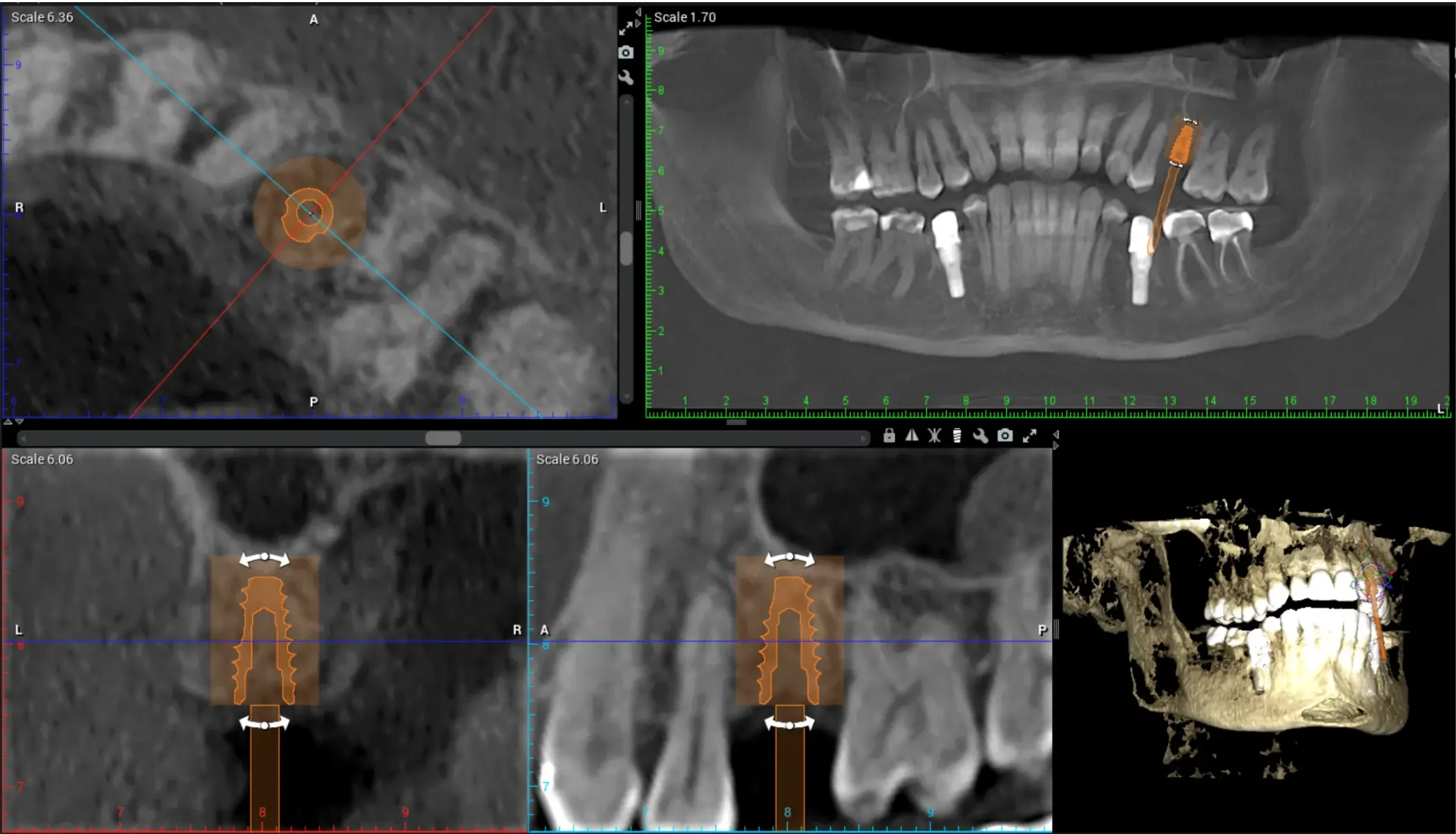
A Panoramic image taken from our CBCT Implant Planning Software. We outlined the inferior alveolar nerve in red, which is always a structure to avoid when placing dental implants in the lower jaw.
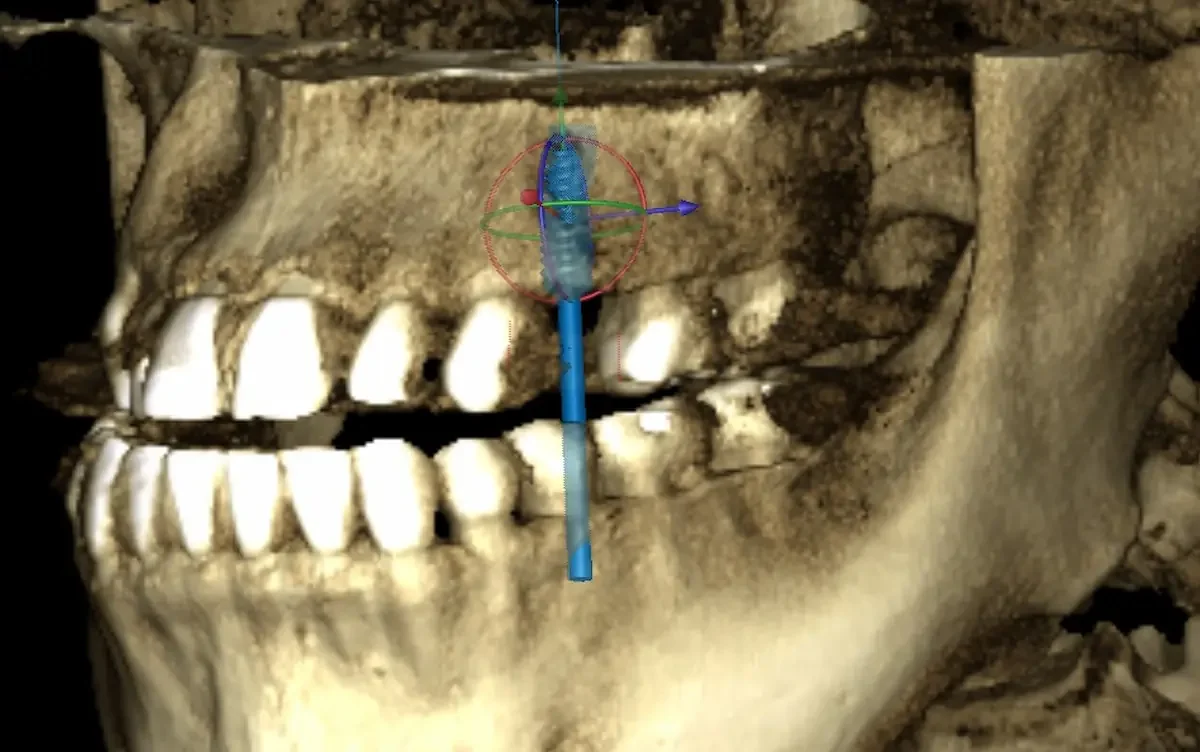
A 3D view of where the implant (highlighted in orange) is planned to go in the lower jaw, along with the inferior alveolar nerve in red. This view helps show how the bite forces will be directed on the impolant from the upper teeth.
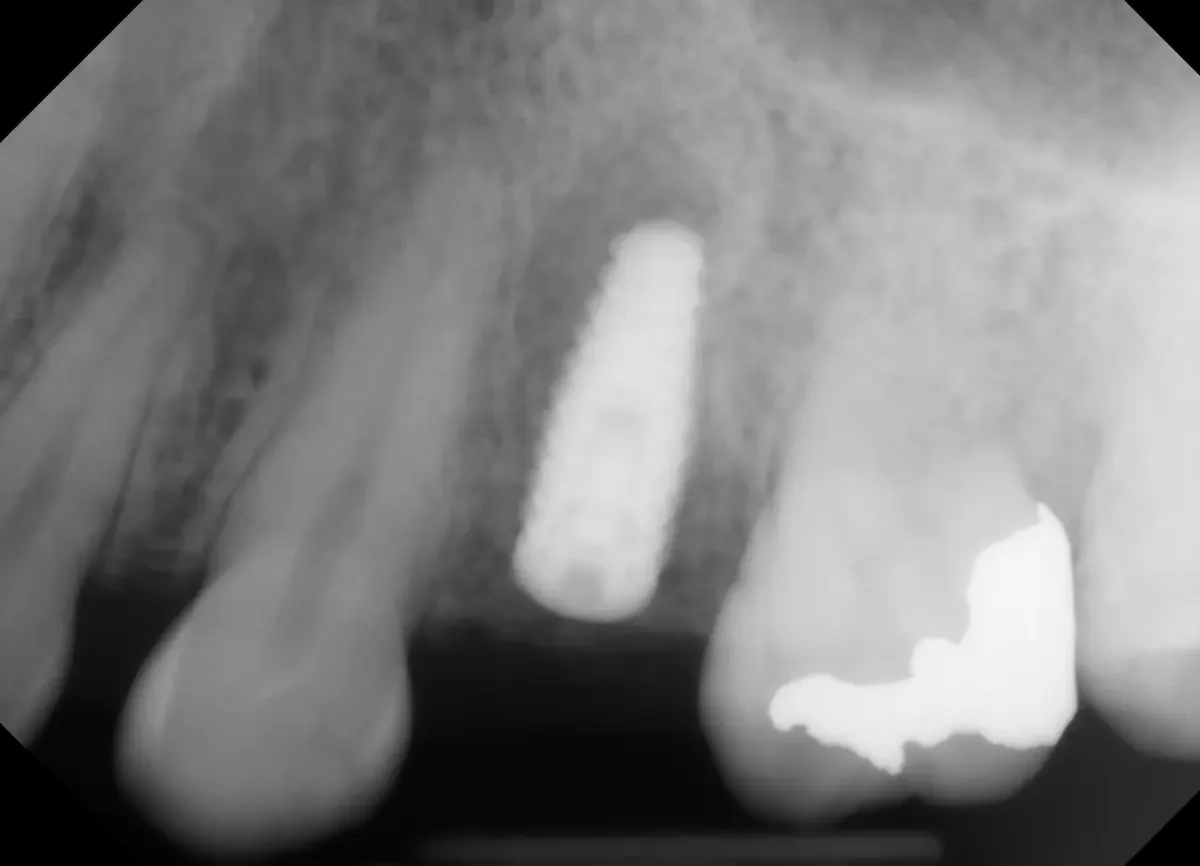
The power of 3D imaging shown. The 2D X ray makes it seem like there is more bone below where the implant was placed. But there is really a ridge making available bone much smaller, which you can clearly see in the right sider of the image. Without a 3D scan, it would have been nearly impossible to know this.
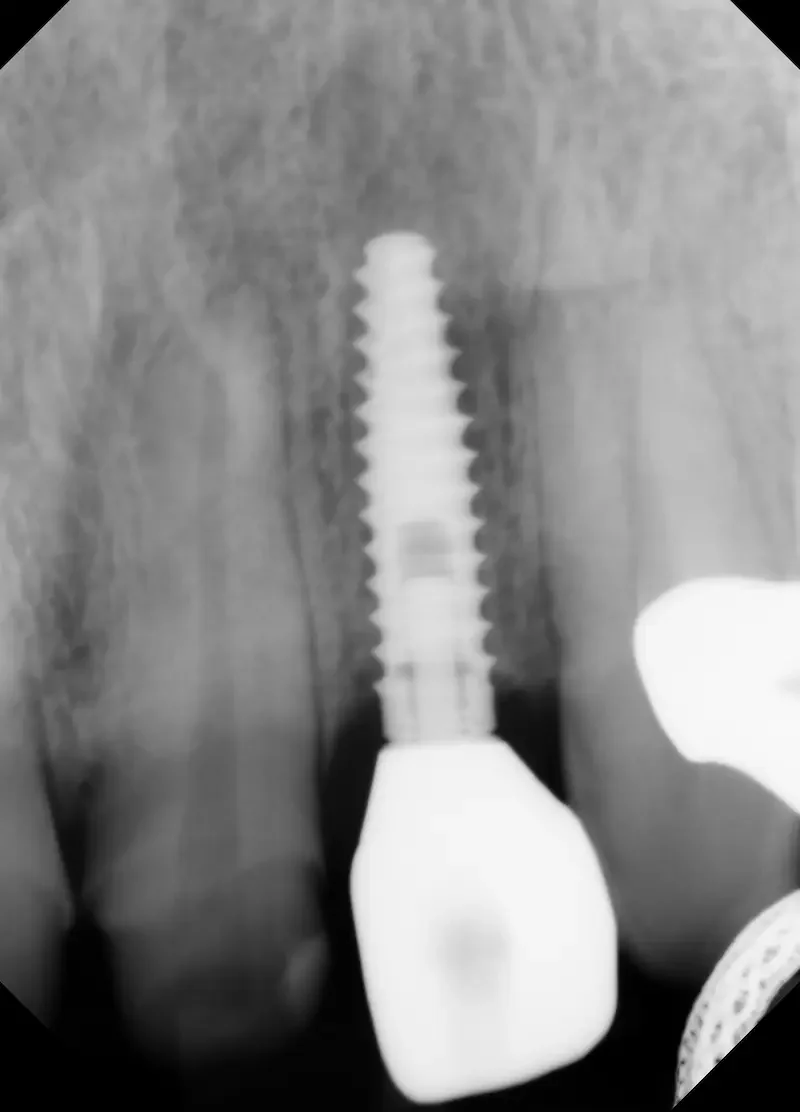
Compare this final X Ray the day of implant surgery with the projected angles in our planning software.
Also notice where the bottom of the implant is. In the 2D X Ray, it seems like there would be more room in the bone below the implant. But we know from our 3D CBCT planning that there is not.
After eight weeks of healing, we took a CBCT scan to measure the bone and plan the implant placement (more detail in the Youtube Video above). These 3D images let us:
Visualize healed bone and ridge contours
Ensure Bone is fully healed
Select the ideal position, angle, and depth for the implant
Precisely plan the case to maximize outcomes
Sometimes incorporate a surgical guide for implant surgery, though we did not use one in this case due to lack of space in the back of this patient’s mouth. Surgical guides are useful but not always necessary.
Eight weeks of healing is a relatively short time for predictable implant placement, and it is often necessary to wait longer. In this particular case, our protocols combined with the patient’s health allowed for a shorter healing timeline. It’s also important to emphasize that instead of focusing solely on placing the implant where there is bone, modern implant planning puts the implant exactly where the final tooth restoration should be — giving the patient the best esthetics and function long-term. The CBCT imaging is vital for that process.
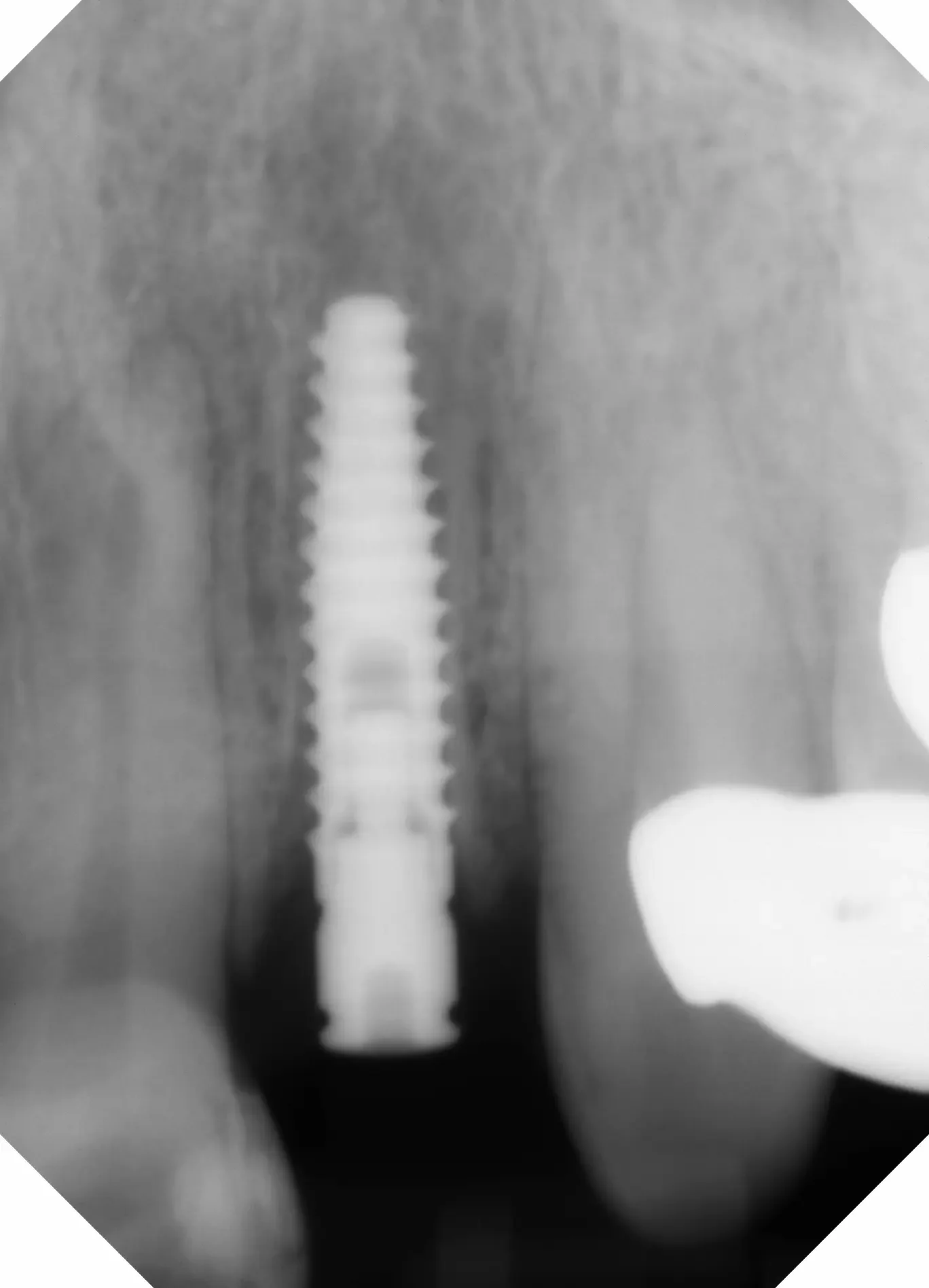
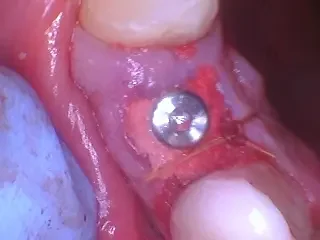
Day of Implant Placement — Healing Cap Placed Over Implant
On the day of implant placement, we used the plan created from the CBCT to place the implant in the exact ideal position. Since the bone was especially strong, the implant was seated with a healing cap, which helps shape gum tissue and protect the site while osseointegration occurs — the biological process where titanium fuses directly with bone. Not all implants get a healing cap the day of surgery. Sometimes it’s necessary to place that later after some bone strength has returned.
The X-ray above shows the implant well-centered in the grafted bone — exactly where we planned it to be for optimal restorative results.
Notice:
The bone prepared by the socket preservation graft creates a stable foundation. This was verified by the CBCT analysis.
A healing cap supports soft tissue for a cleaner emergence profile when the final crown is placed.
Right after implant placement, here is the photo of the implant healing cap and white sutures. The gum tissue is intentionally bunched up on the right side of the healing cap. This allows for more strong, keratinized tissue on the cheek side of the implant, which is protective for the implant’s long term health.
Why The Original Bone Grafting Worked
By preserving bone at the time of extraction and thoughtfully planning implant placement, we help ensure:
✔ predictable osseointegration
✔ better long-term stability
✔ improved esthetics and gum contour
✔ fewer surprises or complications later
The original socket preservation is not required for every extraction — but when an implant is planned, it’s often the smartest long-term choice to protect bone and support future tooth replacement.
What Comes Next in Implant Process?
Right now, this implant is undergoing osseointegration — the process where new bone grows and bonds directly to the implant surface. Once this fusion is strong (usually several weeks), the final implant crown will be fabricated and attached.
Stay tuned for Part 3, where we’ll share:
Final crown placement photos
Before/after comparisons
What the patient can expect for function and esthetics
If you’re curious about your own implant journey — from extractions and grafting to final restorations — we’re happy to walk you through what makes these steps predictable, comfortable, and successful.
Teuscher Legacy Dental — St. Charles, IL
Call or text (630) 762-0000 or visit teuscherdental.com for more information.
What Should a Bone Graft Look Like 1 Month After Surgery?
Find out what a bone graft should look like 1 month post surgery.
Real photos & honest healing expectations — from a surgical case at Teuscher Legacy Dental in St. Charles, IL
Patients Ask Us:
“Is what I’m seeing one month after my extraction and bone graft normal? Is it supposed to look like that?”
About the author
This article was written by Dr. Brayden Teuscher, a general dentist with a surgical focus on tooth extractions, bone grafting, and dental implants in St. Charles, IL, serving Kane County, Campton Hills, Geneva, Elburn, and surrounding communities.
At Teuscher Legacy Dental, we place extraction socket preservation bone grafts every week. The 1-month mark can be a major milestone — usually, soft tissues have mostly healed, bone formation is continuing under the surface, and discomfort should be minimal. But patients often aren’t sure what “normal” healing looks like at this stage.
In this post, I’ll walk you through:
What normal 1-month bone graft healing should look like
Real photos from a current patient case
What we evaluate clinically at this stage
When you might need to be seen sooner
Case Overview: Why This Bone Graft Was Done
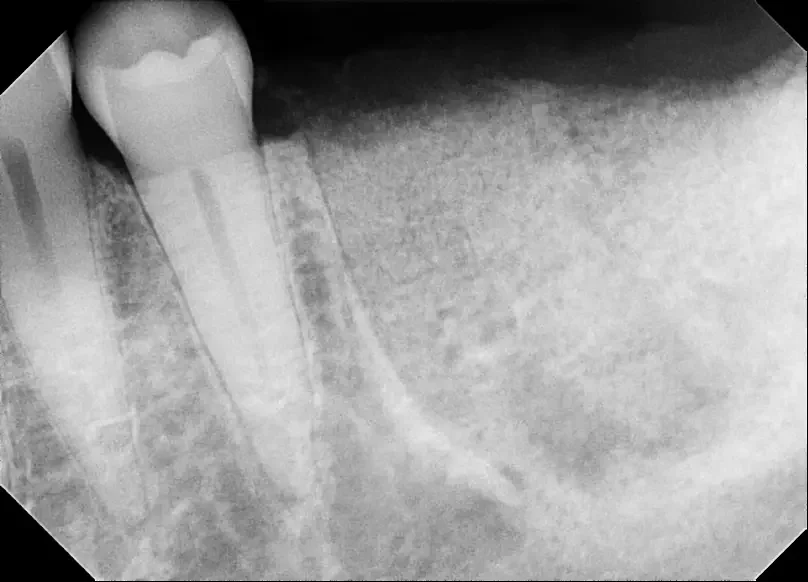
Tooth #13 (center of X Ray) had an old root canal that was infected. In the 2D X Ray, the infection is difficult to see.
The CBCT 3D slice clearly shows the dark infection around the edge of the root. To the right side, a previous extraction site not done in our office.
This patient is a female in her 60s. In the 2D X Ray above, the tooth #13 doesn’t seem so bad. But in the 3D CBCT scan to the right, we can clearly see an infection around the root from the old root canal. This patient did not want to re-do the root canal, and preferred to have the tooth extracted and socket preservation bone graft placed to prepare for future dental implant.
*Notes for this case: The CBCT imaging on the right allows us to see things we never would have known about from a 2D X Ray. Notice how clearly you can see the abscess in the CBCT slice. CBCT imaging in dentistry is the standard of care for implant planning, and an incredibly powerful diagnostic tool when evaluating for infection and other conditions.
Also, This patient had an infected tooth #14 extracted and a collagen base bone graft placed at another office about 2 months before seeing us. That is the darkness on the right side of the X Ray and CBCT screenshot above. This type of bone graft heals more slowly and often less predictably than the demineralized bone particles we most often use. I did not take a picture of this particular site that day since we were evaluating the tooth #13 in front of it. At our office, we use that same collagen base graft in certain select situations. That isn’t the point of this particular post, but worth noting.
The Extraction and Socket Preservation Procedure Day
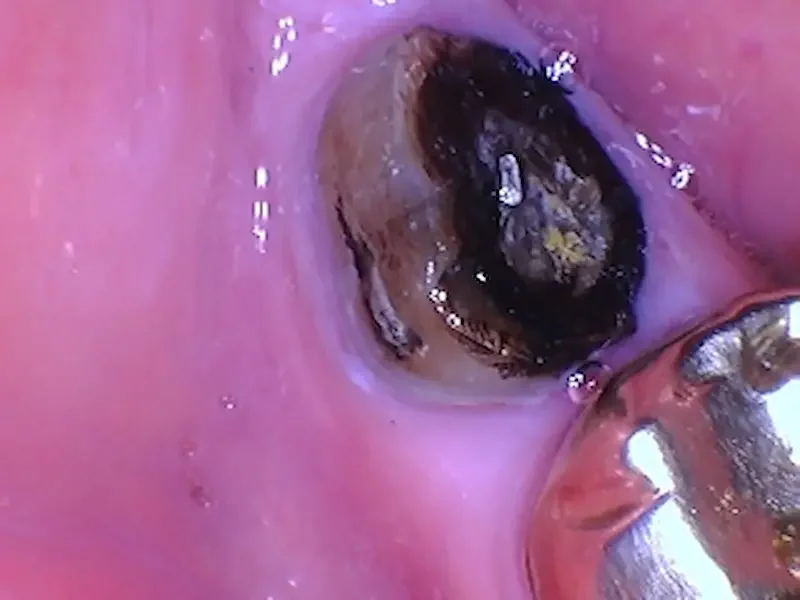
After the tooth was extracted and bone graft placed. Notice how bone particles fill the previous root and infection space.
Photo of the collagen plug and white sutures over the bone particle graft. You can see some of the bone particles over the top of the collagen. It is normal for some of the particles to spill out at first.
In the X Ray above you can see the tooth socket filled with bone graft material. (Our graft is center of X Ray, right next to the tooth that is still there. To the right of center is a larger infection that was previously grafted at a different office using different materials.) In the photo, You can see the pink collagen plug, white sutures that criss-cross over the top, and even some gray bone particles that spilled out onto the collagen. This is normal and the grafted site looks great!
Our method of using demineralized particulate bone with a collagen plug and sutures over the top helps by:
Preserving alveolar ridge (jaw bone) width and height
Supporting new bone formation
Protecting the graft site while soft tissue heals
Extraction and bone graft procedures are quite routine at our office, and this case is a good example of what happens.
What Real Healing Looks Like at 1 Month
One month after procedure, the pink gum tissue is almost fully closed. The darker red area is immature gum tissue. The light pink on the outside is healthy. If it was infected it would be much redder and more swollen.
One month later, our patient was doing great. In general, the way a bone graft site looks after one month can vary dramatically based on patient factors like age, medical history, current medications, smoking status, and the extent of tooth infection prior to extraction. But this picture should give you a good idea of what to expect.
At 1 Month, we see Soft Tissue Progress
By 4 weeks after surgery you should see:
Gum tissue mostly closed over the grafted site
A smooth contour of healed soft tissue
Little to no visible crater
Minimal redness or swelling
This means the gum has largely healed on the surface and your body is moving into deeper phases of bone rebuilding.
Clinically, this is great healing. If the soft tissue border looks pink and stable without irritation, that’s exactly what we want to see.
Bonus: What An Extraction and Bone Graft Site Should Look Like:
What’s Happening Under the Surface at 1 Month
Even if it “looks all the way healed,” real bone growth is still happening deep inside:
The graft material is acting as a scaffold for new bone cells
True bone mineralization continues for months, not days
At 1 month, early bone formation is already underway but will continue strengthening
This matches typical bone graft healing timelines described by peer reviewed surgical literature, where bone integration usually spans weeks 2–6 and beyond.
So if the site seems flatter, closed, or even slightly irregular — that’s normal. The surface has healed; the bone is still maturing.
How It Should Feel at 1 Month
Most patients report:
Little to no discomfort
Occasional slight pressure or tightness
More confidence chewing elsewhere — and not thinking about the graft site
By this stage, most pain has resolved and you should feel pretty normal. Some sensitivity is okay, but sharp or worsening pain isn’t. Increasing pain or swelling in that area can indicate infection.
When Healing Isn’t Typical
Contact your dentist if you notice:
Increasing pain or throbbing
Swelling that worsens after initial improvement
Foul taste, active drainage, or pus
Fever or feeling unwell
These are not typical at one month and may need evaluation.
Final Takeaway
At 1 month after a bone graft, your site should look healed on the surface, feel comfortable, and show at least some pink, stable gum tissue.
Deeper bone healing is still in progress — and that’s exactly how it should be.
Healing isn’t “instant perfection” — it’s progress. If you’re not sure whether your graft is healing normally, we can help evaluate and reassure you.
Have Questions or Want Your Site Evaluated?
Call us at (630) 762-0000 or request a surgical evaluation at Teuscher Legacy Dental in St. Charles, IL.
Healing isn’t always pretty — but knowing what’s normal makes it a lot less stressful.
— Dr. Brayden Teuscher
What Does an Extraction & Bone Graft Look Like 2 Weeks After Surgery?
Real Photos & X-Rays From a Surgical Case in St. Charles, IL
One of the most common questions we hear from patients after a tooth extraction and bone graft is:
“Is this what a bone graft is supposed to look like at 2 weeks?”
At Teuscher Legacy Dental in St. Charles, IL, we perform extractions and bone grafts all the time, and the 2-week mark can be a critical checkpoint. It’s often when the slowest healing patients feel better — but still worry that something doesn’t look “right”.
In this post, I’ll walk you through:
What normal healing looks like 2 weeks after extraction and bone graft
Real before-and-after photos and X-rays
What we evaluate clinically at this stage
When we’re reassured — and when we’re concerned
This is a real case from our surgical practice, not a stock example.
About the author
This article was written by Dr. Brayden Teuscher, a general dentist with a surgical focus on tooth extractions, bone grafting, and dental implants in St. Charles, IL, serving Kane County, Campton Hills, Geneva, Elburn, and surrounding communities.
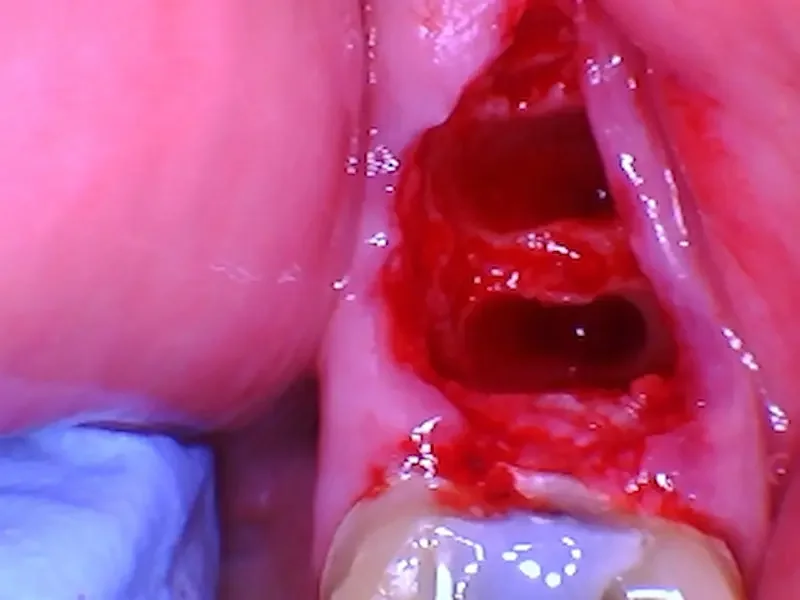
Case Overview: Why This Tooth Needed Extraction & Bone Grafting
A lower right molar crown fell out. The darkness is mostly stain, but there are small areas of decay that likely contributed to the crown loosening. The tongue side of the remaining tooth is flush with the gums.
The inside of the crown that fell out. Some old cement came out with the crown.
An X-Ray of tooth #31 with crown missing. You can see this tooth had a previous root canal and large post in the back root.
This patient is a female in her 60s. She patient decided to have this tooth removed due to structural compromise that made long-term restoration unpredictable. Not everyone decides to get their tooth out, but this patient did. Because the patient is planning for a future dental implant, a socket preservation procedure with a bone graft was performed at the time of extraction.
Surgical goals of the bone graft:
Prevent collapse of the socket during early healing
Create a stable foundation for future implant placement
This was a routine procedure for us at our surgical practice. We extracted the tooth, then filled the root spaces with a 70/30 ratio cancellous to cortical cadaver bone particulate graft. Next we stabilized the graft with a collagen plug and suture to support predictable bone regeneration. Photos below:
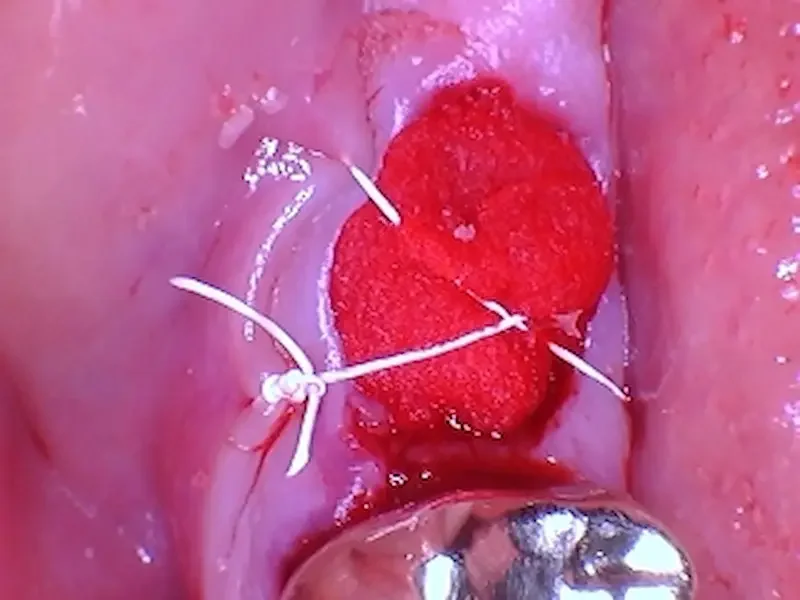
A photo of the grafted site. The red part is the collagen plug over the top of the particle graft. In this case one figure 8 suture was enough to keep everything stable for healing.
An X-Ray of the extraction site after bone graft placement. You can see how the lighter shade of the grafted particles fills in the space where the tooth roots were before the extraction.
What We Look for Clinically at the 2-Week Healing Mark
At two weeks, bone has not yet fully regenerated — and that’s important to understand.
This phase is primarily about soft tissue stability and graft protection.
At 2 weeks, we evaluate:
Whether the graft material has remained stable (versus completely fallen out)
How the gum tissue is closing over the site
Signs of inflammation or infection versus healthy healing
Whether the site is protected enough to continue healing undisturbed
This is often the visit where patients expect the site to “look filled in.” That usually does not happen yet — and that’s normal.
Real Photo: What You’re Seeing at 2 Weeks
2 Weeks After Surgery
The grafted site is healing well. The white and yellow granules toward the top of the photo are residual bone graft particles, not an infection. and toward the bottom near the gold crown you can see the gums are already almost fully closed over.
Our patient was concerned about the “yellow spots”. We explained these are particles from the bone graft, NOT an infection. They will likely exfoliate (fall out) on their own, and there is plenty of bone graft underneath them. It is very normal to lose a few of the graft granules, especially the cortical granules which are the bigger and denser particles in the particular mix we used in this case.
A big key that you can see in the photo is that the gum tissue around the site and in the cheek area was pink, and minimally swollen. If an infection were present, we’d see deep red, irritated or visibly swollen tissue. Usually it would be painful. Our patient had no pain.
Some of the gums closer to the gold crown are completely covering the extraction site already, which is great healing for someone in their 60s! Remember that medical conditions can affect healing timelines, so sometimes even for a younger person, healing this good doesnt happen for another week or two.
To sumarize:
The gum tissue has migrated inward and downward, almost fully closing the extraction socket
The socket appears shallower, but not closed
Mild surface irregularity is expected
This is normal healing.
True and final bone maturation occurs months later, not weeks.
Is It Normal for a Bone Graft to Look Hollow at 2 Weeks?
Yes — and this is one of the biggest misconceptions we get asked about.
At two weeks:
The body is still forming early connective tissue
New bone has not fully mineralized yet
The graft is acting as a scaffold, not final bone
If the site looked “fully filled in” at two weeks, that would actually be unusual.
Bonus content: What a bone graft should look like after 1 week healing.
Should There Still Be Discomfort at 2 Weeks?
Most patients report:
Minimal soreness or pressure
No sharp or worsening pain
Improved chewing comfort, especially on the opposite side
Pain that increases after week one is not typical and should be evaluated.
How We Know This Graft Is Healing Normally
From a surgical standpoint, this site shows:
Stable graft material
Healthy soft tissue color and contour
No signs of infection or graft loss
At this point, we’re looking for progression, not perfection.
Warning Signs That Are Not Normal at 2 Weeks
While most bone grafts heal uneventfully, contact your dentist if you notice:
Increasing pain after initial improvement
Persistent swelling or pressure
Foul taste or drainage
Fever or systemic symptoms
Early evaluation can prevent larger complications. When these symptoms are present, an infection is possible.
What Happens Next in the Healing Timeline?
Typical progression:
Weeks 0–2: Soft tissue stabilization
Weeks 3–6: Early bone formation begins
3–6 months: Bone matures and strengthens
Implant planning: Based on graft size and location
Every case is different — this is why follow-up matters. At our practice, each surgical case is unique and patients get custom treatment timelines depending on their unique needs.
Unsure If Your Bone Graft Is Healing Normally?
Many patients come to us worried — and leave relieved after we review healing clinically and on X-ray.
If you’ve had an extraction or bone graft and:
Something doesn’t look right
Healing feels slower than expected
You want a second opinion before implant placement
We’re happy to evaluate your site and give you a clear, honest assessment.
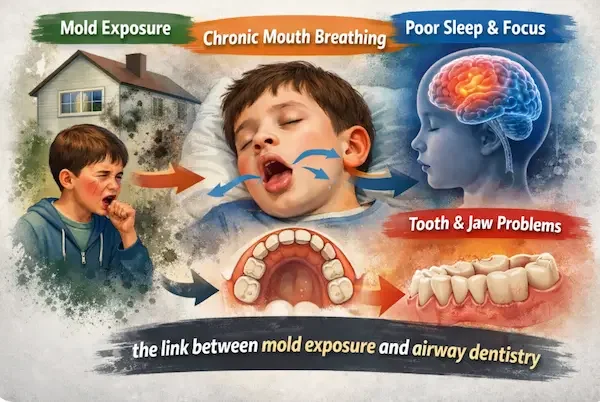
Mold Exposure, Mouth Breathing, and Why Airway Development Matters More Than Cavities
From a Dad and an Airway Dentist…
Myself and my family around the time we discovered the mold in our home
I’m writing this not only as an airway dentist, but much more importantly, as a dad.
My son experienced mold exposure early in life. My wife and I would do anything for our kids! So, like many families, we took the mold exposure seriously:
We identified and extensively remediated the mold source in our home
For over two years, we’ve focused on my son’s gut health and immune support through a pediatric functional medicine practice.
His supplement regiment and food restrictions are exhausting and expensive! But we’ve stayed the course. And yet, he continues to deal with eczema. You may have had a similar experience.
If you’re a parent reading this, you may be wondering:
“We handled the mold—why are symptoms still lingering?”
This article exists because there is often another piece of the puzzle for growing children that goes unaddressed—one that lives in the airway, jaws, and mouth.
Step One: Mold Exposure Must Be Addressed First
When mold exposure is suspected, identifying and dealing with the source is always step one.
This may involve:
Addressing water damage or hidden moisture
Improving indoor air quality
Professional remediation when indicated
No dental, medical, or supplement-based approach can fully work if exposure continues.
Step Two: Immune & Microbiome Support Often Helps
Many families pursue:
Gut and microbiome support
Immune system regulation
Anti-inflammatory nutrition and supplementation
This work—often guided by functional or integrative medicine providers—is incredibly important.
However, even when these steps are taken, many children still struggle.
Why?
Mold Exposure Often Leads to Mouth Breathing
Mold exposure can cause chronic nasal inflammation, even when allergy testing is negative.
When nasal breathing becomes difficult—especially during sleep—children adapt by:
Opening their mouth at night
Lowering the tongue from the palate
Relying on mouth breathing for oxygen
This is not a bad habit.
It’s a protective response.
But over time, this adaptation can affect jaw growth, airway development, and sleep quality.
Bonus: Another factor that influences mouth breathing can be tongue ties. I wrote extensively about that here.
Why Mouth Breathing Affects Jaw and Airway Growth
Proper facial and airway development depends on:
Even with an extensive supplement list and mold removed, my son still struggles with eczema. Thankfully, he’s still a happy dude!
The tongue resting on the roof of the mouth
Gentle outward pressure that widens the upper jaw
A nasal airway that develops alongside the jaws
With chronic mouth breathing:
The tongue rests low
The upper jaw grows narrow
The palate becomes high and vaulted
The nasal airway becomes smaller
This creates a cycle:
Narrow jaw → restricted airway → worse nasal breathing → more mouth breathing
Long-Term Consequences of Mouth Breathing in Children
1. Jaw & Facial Development (Including Appearance)
Chronic mouth breathing during growth is associated with:
Narrow jaws
Crowded teeth
Recessed or underdeveloped jaws
Longer, less balanced facial growth
This is not about vanity—it’s about structure, airway space, and long-term function.
Beauty isn’t necessarily the goal (brain development is. See below.) But it is true that healthy = beautiful. Notice the difference in jaw development in the picture below.
Henry Cavill has a well developed jaw. He is a nose breather! But Napolean Dynamite is notorious for his open mouth and inattention at school!
2. Sleep, Brain Development & Behavior
Healthy brain development requires deep, restorative sleep.
Research shows associations between pediatric sleep-disordered breathing and:
Attention difficulties
Hyperactivity or ADHD-like symptoms
Learning and emotional regulation challenges
Mouth breathing does not cause ADHD—but it can worsen attention and behavior, especially during critical growth periods.
3. Oral Health & the Microbiome
Mouth breathing can also lead to:
Dry mouth at night
Altered oral microbiome balance
Increased cavity risk
Inflamed gums despite good hygiene
Cavities are often a signal of airway dysfunction, not the root problem.
The Key Takeaway for Parents
Cavities matter.
But airway development, jaw growth, and sleep quality matter way more. That’s the perspective of an airway dentist.
Even after mold exposure is addressed and immune support is underway, dental airway evaluation may still be necessary. We always emphasize partnering with functional medicine practitioners and myofunctional therapists!
➡️ In the next post, we explain exactly what an airway dentist evaluates—and what parents can expect…
🎄 The Worst Holiday Treat for Your Teeth
One of my favorite snacks. Perfect with those holiday family movie nights… What is the most frequent holiday treat source of tooth issues?
Unfortunately, it’s popcorn 🍿
Every holiday season, we see patients who cracked a tooth on an unpopped kernel or ended up with a sharp popcorn shell wedged deep under the gums. Those thin hulls are rigid, sharp, and perfectly shaped to irritate gum tissue and cause inflammation—or even infection—if they get stuck.
Popcorn feels light and harmless, but your teeth (and gums) pay the price.
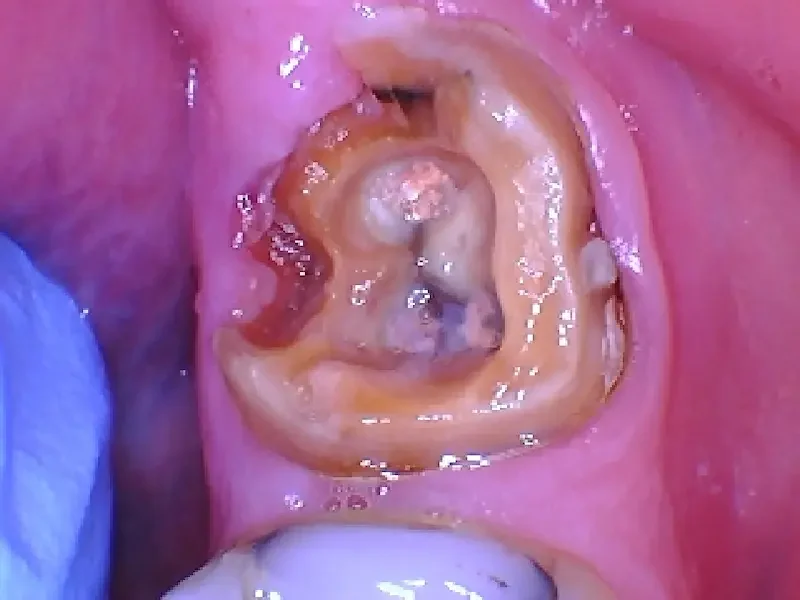
Here’s a real case from last week:
Gum irritation causing the patient lots of pain over the last couple days. We got her numb and cleaned out the area.
The culprit causing the gum pain!
After we fished out this popcorn kernel, our patient felt much better!
If you love popcorn:
Avoid crunching unpopped kernels
Floss gently if a shell gets stuck (sooner than later, so it doesn’t lodge itself deeper!)
Call or text us if irritation lasts more than a day or two… we can get it out
We hope your teeth make it through the holidays intact 😄
Merry Christmas and Happy New Year from Teuscher Legacy Dental!
What Does an Extraction Bone Graft Look Like 1 Week After Surgery?
Edited February 4th, 2026
One of the most common questions patients ask after a tooth extraction with a bone graft is:
“Is this what it’s supposed to look like?”
If you’re about one week out from an extraction and bone graft, this article will show you exactly what normal healing looks and feels like, using real patient clinical photos from our St Charles, Illinois dental practice.
Quick orientation: Where You’re at 1 Week Post Op (Bone Graft Healing Timeline)
Days 1-3: Blood clot, swelling, early inflammation
Week 1: Granulation tissue forms (what you’re seeing now)
Weeks 2–3: Gum tissue strengthens, color normalizes
Months 1-4: Bone begins to consolidate
Months 4–6: Implant readiness (case dependent)
About the author
This article was written by Dr. Brayden Teuscher, a general dentist with a surgical focus on tooth extractions, bone grafting, and dental implants in St. Charles, IL, serving Kane County, Campton Hills, Geneva, Elburn, and surrounding communities.
Why This Tooth Needed an Extraction and Bone Graft
This case involved tooth #19, a lower molar that had a large infection caused by a crack on the back (distal) side of the tooth.
Before the tooth was removed, there was a draining sinus tract, which means the infection had been present long enough that the body created a small channel to release pressure and bacteria.
X Ray before Extraction. Notice the darker area around the roots of the molar- that’s where the infection is.
Picture of the back side of the tooth. Notice the crack in the center of the tooth. This is the infection’s source. And the pimple to the right side is where the pus from the infection is draining out of the gums.
Once the tooth was removed, the infected tissue inside the socket was physically cleaned out. This step is critical—bone grafts only work when infection is thoroughly removed first. The long term plan is to replace this tooth with a dental implant. We do this all the time for patients in Kane County, Illinois. An antibiotic was also prescribed after surgery to support healing once the infection source was eliminated.
Not every tooth extraction requires a socket preservation bone graft. And, at one week, the grafted site is far from fully healed. In fact, while socket preservation reduces alveolar ridge bone collapse, bone remodeling and maturation still continues for months, but the evidence is clear socket preservation maximizes the chances at maintaining bone volume (Byrne GJ et al. Socket preservation of implant sites — Journal of the American Dental Association (JADA). 2012)
What Type of Bone Graft Was Used?
After cleaning the socket, a bone graft was placed to help preserve bone and support future healing.
In this case, the graft included:
70/30 cancellous to cortical bone particulate
Cancellous bone helps new bone form more quickly
Cortical bone helps maintain strength and volume
A collagen plug placed on top of the graft
A PTFE suture in a figure-8 pattern to hold everything stable
This is a very common approach after extracting an infected molar, especially when preserving bone for possible future implant placement.
X Ray showing where the tooth used to be, now filled with bone graft particles after extraction at Teuscher Legacy Dental.
Photo immediately after extraction and bone graft. The shiny red is a collagen material used to help blood clot over the graft. The sutures blend into that material. The draining infection to the right side of the graft was cleaned out physically after the tooth was extracted.
What Does an Extraction Bone Graft Look Like After 1 Week?
One week after extraction and bone graft, the gums are closing over the hole where the tooth used to be. The white appearance inside the crater can be alarming, but it is normal healing of the gum and bone graft. Here you can see the figure 8 of the stitches more clearly. Typically we remove these stitches after 1 week.
At one week post-op, the extraction site looked exactly how we expect healthy healing to look.
Most patients notice:
A small crater or hollow where the tooth used to be
A white or off-white material inside the socket
Gums that are slowly healing inward, but not fully closed yet
That white appearance is normal. It is not pus or infection.
It usually represents:
Healing tissue
Residual collagen material
Early bone formation happening underneath
At one week, the gums are not supposed to be fully closed yet.
How Should an Extraction Bone Graft Feel After One Week?
In this case—and in most similar cases—patients report:
Significant relief once the infected tooth is removed
Mild soreness rather than sharp pain
Gradual improvement each day
Many patients are surprised that they feel better after the extraction than they did before, especially when a chronic infection was present.
Bonus Resources: What Does an Extraction & Bone Graft Look Like 2 Weeks After Surgery?
What Does an Extraction & Bone Graft Look Like 1 Month After Surgery?
Is Pain Normal After an Extraction Bone Graft?
Some soreness is normal, especially during the first week.
For many patients, pain is well managed with over-the-counter medications.
When safe for the patient, a common approach is:
Ibuprofen 400–600 mg
Four hours later: Acetaminophen (Tylenol) 500 mg
Continue rotating every four hours as needed
This combination helps control both inflammation and discomfort without stronger medications.
(Always follow your dentist’s instructions and confirm these medications are safe for you.)
When Should You Be Concerned?
While a crater-like appearance and white healing tissue are normal at one week, you should contact your dentist if you notice:
Increasing pain instead of gradual improvement (especially throbbing pain)
Swelling that worsens after day 3–4
Foul taste or active drainage
Fever or feeling unwell
These are not typical signs of normal healing.
The Big Takeaway: This Is Normal Healing
At one week after an extraction with a bone graft:
The site often looks open
The graft is working underneath the surface
Gums heal slowly and intentionally
Bone regeneration takes months, not days
Healing doesn’t look “pretty” early on—but that doesn’t mean something is wrong.
Remember, that healing will take a matter of months. But it’s often worth the wait: Studies indicate significant long-term positive effects on alveolar ridge height and volume when socket preservation is used compared to extraction alone (Atieh MA, Alfardan L, Alsabeeha NHM, et al. Alveolar ridge preservation after extraction: systematic review and meta-analysis. PubMed. 2022).
If you’ve been told you need a bone graft or you’re wondering whether your extraction site looks normal, these are exactly the kinds of questions we want patients to ask. In our St Charles, Illinois dental practice, we hear these questions all the time.
Clear answers reduce anxiety—and better understanding leads to better healing.
If you’re in the Kane County, IL area, come see us for a free consult!
P.S. - If this blog was helpful, what else would you like me to write about or show? Message on FB or IG… links below. Thank you!
The Truth About Same-Day Extractions and Implants in St. Charles
Everyone loves the idea of walking in with a broken tooth and walking out with a dental implant the same day. It sounds efficient, high-tech, and convenient — and sometimes, it really is.
But here’s the truth most people never hear:
same-day dental implants are a phenomenal option in the right situation… and a costly mistake in the wrong one.
At Teuscher Legacy Dental in St. Charles, IL, we place and restore dental implants every week — including immediate-placement (“same-day”) cases. The key is knowing when it’s the smart move and when patience leads to better long-term success.
What “Same-Day” Actually Means
“Same-day dental implants” (also called immediate implant placement) means the implant is placed at the same appointment as the tooth extraction.
Sometimes a temporary crown or healing cap is attached right away, giving you the appearance of a new tooth while the implant integrates beneath the surface.
That’s very different from “same-day final teeth.” True final restorations still require a healing period — usually several months — for the bone to bond securely to the implant.
So the real question isn’t “Can you place an implant right away?”
It’s “Will that implant heal predictably and last decades?”
Before Extraction
After Extraction, Same Day Implant in root socket
Picture of same day implant and healing cap sticking out of gums
X Ray of final crown over immediate dental implant
✅ When It’s a Genius Move
Same-day implant placement works beautifully when a few key conditions are met:
Healthy bone surrounds the tooth being extracted
No active infection in the gums or bone
Thick, healthy gum tissue for stability and aesthetics
Excellent primary stability (the implant locks in firmly)
Precise digital planning — guided by 3D CBCT imaging
Here’s an example from one of our recent cases (see images above!):
A patient had a broken down front tooth. Because the surrounding bone and gums were perfectly healthy, we used a fully guided surgical approach to remove the tooth and place an implant in the same visit. The patient left with a custom temporary that looked completely natural — and never had to go a single day without a smile. Dr Brayden Teuscher did a much more thorough case breakdown here.
That’s when same-day is a genius move.
❌ When It’s Not Worth the Risk
Not every extraction site is ready for an implant right away. In some cases, placing too soon can actually set you back — leading to bone loss, infection, or implant failure.
We don’t recommend same-day placement when:
There’s infection or abscess near the root
The bone is too thin or fragile to stabilize an implant
Gum tissue is receding or damaged
Sometimes if you smoke or have uncontrolled diabetes
Could an implant technically go in that day? Maybe.
Should it? No.
At Teuscher Legacy Dental, our primary goal isn’t usually to get the implant done fast — it’s to do it right. If we need to rebuild the bone first, that extra healing time protects your long-term success. Of course, we’d go over risks and benefits of each option, because it’s not always black and white!
Why Planning Beats Speed Every Time
Speed means nothing without stability. That’s why we rely on:
3D CBCT imaging to evaluate bone in every dimension
Digital surgical guides for perfect placement
In-house implant surgery and restoration, so every phase aligns under one plan
When you’re working with a team that performs extractions, bone grafts, and implant restorations under one roof, like we do at Teuscher Legacy Dental, every decision serves the long game — not just the quick win.
We can still streamline care when the conditions are right, but never at the expense of the implant’s lifespan.
What to Expect: Cost, Healing & Comfort
In most cases, same-day dental implants cost about the same as traditional implants. The difference mostly lies in timing, not price.
Healing time: Soft tissue typically heals in 2–3 weeks; bone integration takes 3–6 months.
Comfort: With modern anesthesia and guided precision, most patients report less discomfort than expected.
Aesthetics: You’ll often leave with a temporary tooth that looks natural while healing.
When planning correctly, the process is efficient and predictable — not rushed.
Honest Answers to Common Questions
Are same-day implants safe?
Yes — in healthy, well-planned cases. The risk rises when infection or bone loss is ignored.
How long do same-day implants last?
With proper planning and maintenance, the longevity is identical to traditional implants: decades of function and confidence.
Do they hurt more than regular implants?
Not at all. In many cases, recovery feels even easier because we minimize surgical steps and trauma.
The Bottom Line
Same-day dental implants can be a great tool and shorten dental implant timelines! But not if corners are cut.
When the foundation is healthy, they save time and preserve bone. When it’s compromised, waiting — and rebuilding — is the wiser move.
At Teuscher Legacy Dental, our philosophy is simple:
We plan for forever, not just for fast.
But when we can achieve predicatble, long term results with an immediate dental implant, that’s awesome!
If you’ve recently lost a tooth or are facing an extraction, schedule a 3D implant consultation with our team. We’ll show you exactly what your bone looks like, whether same-day placement is possible, and what path gives you the best long-term result.
Teuscher Legacy Dental
40W131 Campton Crossings Dr, St. Charles, IL 60175
📞 (630) 762-0000 | teuscherdental.com
Award-Winning Cosmetic & Implant Dentistry in St. Charles IL
Why Your Teeth Are More Sensitive In Winter
Ever notice your teeth ache when you step outside on a cold day? In this short video, Dr. Brayden Teuscher explains why: breathing cold air through your mouth can chill the teeth and irritate tiny nerve endings inside them.
Cold, dry air can also inflame the sinuses, which press against upper tooth roots and make them feel sore—even if there’s nothing wrong with the teeth themselves. Especially if you have a mild illness or COVID.
If you deal with seasonal tooth sensitivity, try breathing through your nose, using a soft-bristled brush, and scheduling a check-up to rule out enamel wear or gum recession.
Watch below for a quick explanation and simple ways to protect your teeth this winter. See You Soon!
Confidence Restored with Same-Day Full Arch Implant Rehabilitation
Meet one of our real patients: A professional who came to us with failing upper teeth, frequent discomfort, and a mounting hesitation in business settings because of his smile. His case is featured on another blog post: full arch implants explained. On a single transformative day, he underwent full-mouth extraction of the upper arch and immediate placement of a fixed-on-implants prosthetic (“same-day teeth”) using the advanced arch-restoration protocol commonly referred to as “All‑on‑X”. The lower jaw is up next, completing the full-mouth rehabilitation journey.
What happened
Extraction of all remaining upper teeth in one surgical visit.
Placement of multiple implants in the upper arch, angled & planned for optimal support and immediate loading.
Attachment of a fixed provisional full-arch prosthesis the next day (less than 24 hours later), enabling immediate function and aesthetics.
Detailed surgical and prosthetic planning, digital workflows, and coordination to deliver same-day outcomes with strong functional and cosmetic results.
(For background on how full-arch implant rehabilitation works and the key benefits, see another full case breakdown here.)
Why it matters
Function: The patient regained chewing ability and speech confidence almost immediately, rather than waiting months for healing and final prosthetics. Full-arch fixed implants offer a vastly more stable bite compared to removable dentures.
Aesthetics: Missing, decayed, or failing teeth can undermine a person’s professional presence and self-image. By restoring a full fixed smile, this patient no longer hides his teeth when speaking, presenting, or engaging in meetings.
Psychology & business impact: Confidence in appearance translates into presence in business settings. Our patient noted that after the procedure, he walked into his next client meeting without self-consciousness about his smile. This kind of outcome is especially meaningful when your work requires communication, leadership, or public interaction.
Efficiency: By doing the upper arch and same-day loading, we streamlined the treatment experience. Patient downtime, inconvenience, and emotional burden are reduced when the process is efficient and predictable.
Looking ahead
The lower jaw phase is scheduled and will complete his full-mouth fixed restoration. Post-care will include:
Monitoring implant integration and prosthetic fit.
Hygiene and maintenance of the fixed prosthesis (cleaning under the bar, proper recall).
Long-term support for the restoration’s success and the patient’s overall oral health.
It’s critical to point out that while these full-arch fixed solutions are life-changing when done appropriately, patient selection, proper planning, skilled surgical and prosthetic execution, and maintenance are all vital. Some warnings exist in the literature about over-aggressive extraction and blanket promotion of full-arch implants when less-invasive or preservative options may suffice.
Want to learn about your options?
Schedule a Free Consultation with our Expert Team!
2 Veneers → A Wedding-Ready Smile! (Fast Cosmetic Fix Before the Big Day)
Sometimes the biggest transformations come from the smallest, most strategic changes.
Sally came to us hoping for a brighter, more confident smile before her upcoming wedding — but her timeline was tight. Instead of recommending a full cosmetic overhaul, we focused on what would make the biggest impact quickly: two carefully crafted porcelain veneers.
These veneers restored balance, symmetry, and brightness to her smile without aggressive treatment or multiple lengthy appointments. The result? A natural, wedding-worthy smile that photographed beautifully and felt completely like her.
If you’re considering cosmetic dentistry — whether for a wedding, graduation, or simply because you’re ready for a change — you’d be surprised what a small number of well-designed veneers can do.
Ready to explore your own options?
👉 Book a free cosmetic consultation
A Broken Tooth Solved! Cosmetic Dentistry Explained
When you break a tooth and need a quick, (but beautiful and cosmetic!) fix, what do you do?
See Teuscher Legacy Dental of course!
This patient had a broken tooth and adjacent tooth that was cracked and too yellow. We used advanced, minimally invasive techniques to improve the color and strengthen the teeth in a way that will last. Our patient was thrilled!
Get more detail in the video above.
If you have a similar need for cosmetic dental work, see us for a FREE CONSULT!
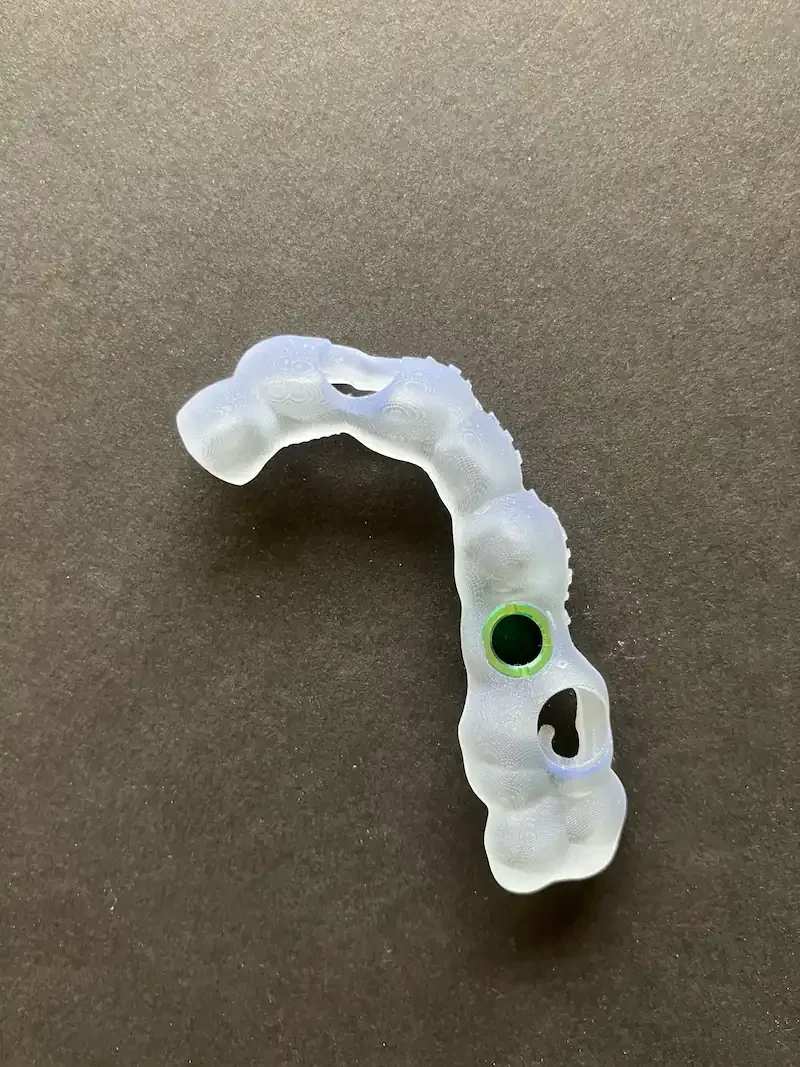
What Are Surgical Guides for Dental Implants — How They’re Made and Used (Real Photos!)
Learn how 3D surgical guides help your implant be placed with pinpoint accuracy. See how Teuscher Legacy Dental plans, prints, and uses them.
What is a Surgical Guide?
A surgical guide is a custom-made template that fits precisely over your teeth or gums during implant surgery.
Think of it like a roadmap — it shows the exact position, depth, and angle where each dental implant should go.
Instead of relying only on visual landmarks or freehand placement, the guide ensures your implant goes exactly where it was digitally planned using your 3D scans.
How a Surgical Guide Is Made
At Teuscher Legacy Dental in St Charles, IL, each guide is made in-house from your Medit digital scan and CBCT 3D X-ray.
Here’s how the process works step-by-step:
About the author
This article was written by Dr. Brayden Teuscher, a general dentist with a surgical focus on tooth extractions, bone grafting, and dental implants in St. Charles, IL, serving Kane County, Campton Hills, Geneva, Elburn, and surrounding communities.
1️⃣ Digital Impression (Medit Scan)
3D digital impression of top teeth to make surgical guide for dental implant
3D digital impression of bite to plan precise bite relationship for final crown BEFORE any implant work is done.
We take a detailed 3D surface scan of your teeth and gums. We have two Medit brand intra-oral scanners at our office. They dont gag you like traditional impression material will!
2️⃣ 3D Bone Scan (CBCT) and Virtual Implant Planning
Your CBCT scan shows the underlying bone volume, nerves, and sinus anatomy.
We plan in more detail where the final tooth will go, and the angle the implant needs to be placed. This data is merged with your Medit 3D intra-oral scan inside our implant planning software. This data is used to 3D print the tooth model and surgical guide below.
3️⃣ Guide Design & 3D Printing
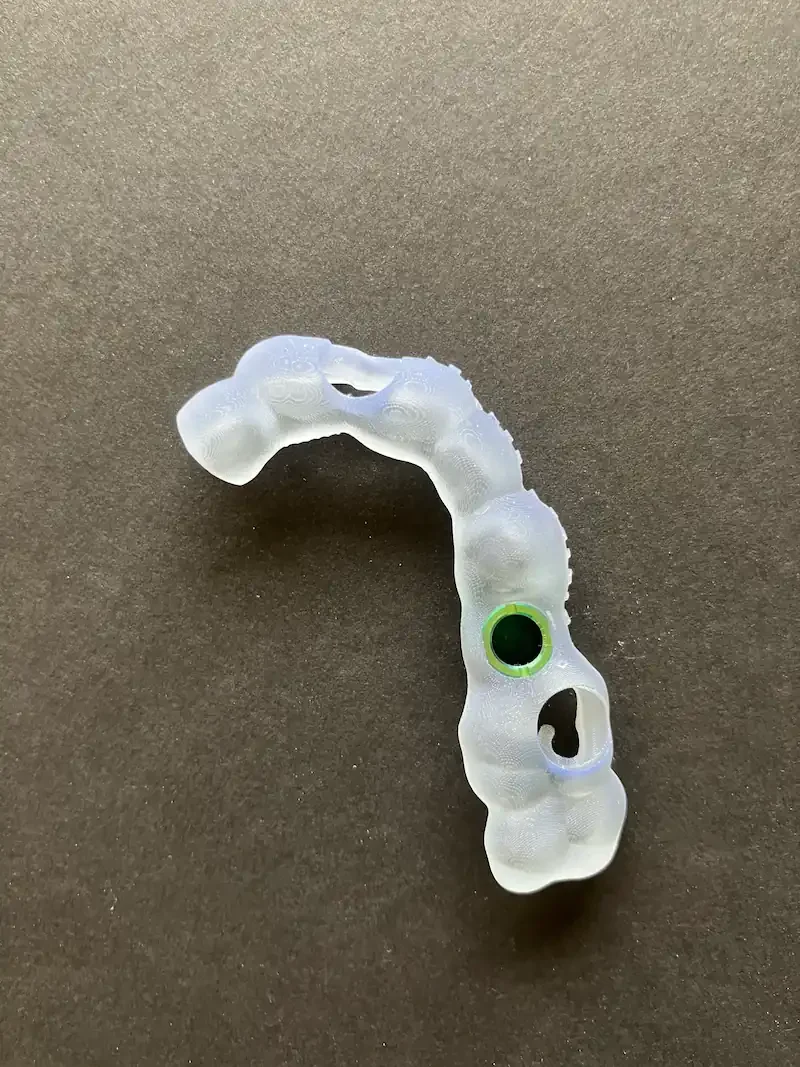
3D printed model of the patient’s upper arch, showing where the implant will be placed
Green metal sleeve only allows the drill to enter bone in one specific direction. This direction is the exact place we decided in the planning phase.
Once the implant and crown plan is approved in the planning software, the surgical guide is designed with metal sleeves to control the drill’s exact path. The file is printed on a dental 3D printer using biocompatible resin and disinfected before surgery.
How the Surgical Guide Is Used During Surgery
On the day of surgery, the guide is seated snugly on your teeth or gums, just like on the initial model.
Each drill step passes through the guide sleeve, keeping your implant trajectory perfectly aligned with the digital plan.
This means:
✅ Smaller incisions and less swelling
✅ Shorter surgery time
✅ Faster recovery
✅ A precisely restored bite that matches your smile design
For patients, this translates to more predictable results and a smoother overall experience.
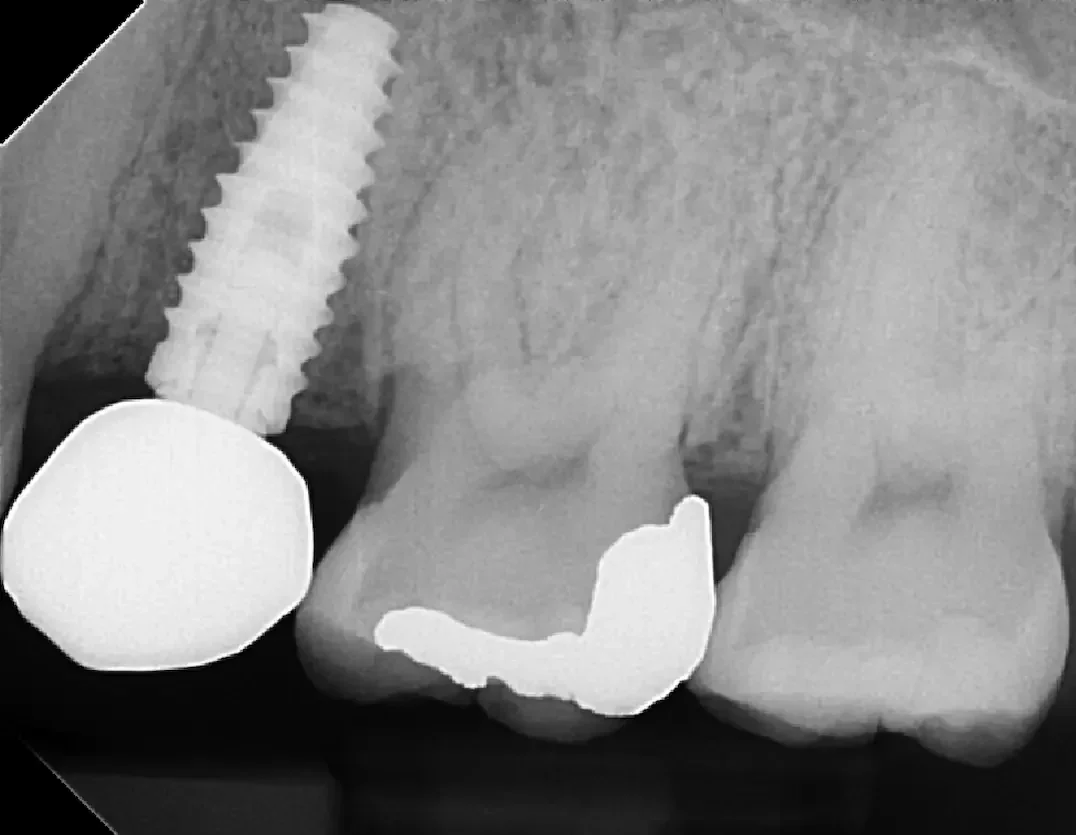
Perfect implant position on surgery day - due to precise planning.
A beautiful final crown that fits perfectly into the patient’s bite - just like we planned.
Why Precision Matters at Teuscher Legacy Dental
Every implant case in our office is planned with BioHorizons implants (most often using Tapered Pro implants) and often using Densah osteotomy protocols — then executed using the same digital plan you see in your consultation.
That consistency creates:
📍 Precision – Implants placed exactly where the restoration belongs
💪 Predictability – More bone contact and less adjustment later
😊 Peace of mind – A precise plan is in place before surgery
Common Questions
Q: Can every implant be done with a guide?
Most can — especially single implants, multi-unit bridges, and full-arch cases. Some immediate extraction sites require slight modification or open-flap visualization, but we still base the surgery on the same digital plan.
Q: How long does it take to make a guide?
Typically 1–3 days from planning to printing.
Q: Is guided surgery more expensive?
Slightly, but it pays off in precision and peace of mind. Most of our implant fees already include guided placement.
Related Reading
Much more info on cost, timeline, and risks of dental implants here: Dental Implants
📍 Serving:
St. Charles IL | Campton Hills | Geneva | Elburn | Fox Valley
💬 Ready to Explore Dental Implants?
Schedule your Free Digital Smile Design & Implant Consult today.
📞 Call (630) 762-0000 or Book Online.
Traditional vs. Snap-In vs. Fixed Implant Dentures: Which Is Right for You?
Introduction: Similar Look, Different Feel
Patients ask us all the time:
“Do I need implants to hold my dentures? Should I get snap-in dentures or fixed implant dentures?”
They all look similar — but the way they fit, feel, and function have key differences.
There are three main paths for replacing a full set of teeth:
1️⃣ Traditional (tissue-supported) dentures
2️⃣ Snap-in (implant-retained) dentures
3️⃣ Fixed implant dentures
I’ve explained in more detail what each denture option is in a separate post. But in general, each has its place. Some of our patients in St. Charles, Geneva, and Campton Hills do great with traditional, tissue-supported dentures — especially on the top arch where soft tissue support is strong. Others want the added confidence, stability, and bite strength that implants can provide, either fixed or snap-in.
If you’ve been told you “need dentures,” this guide will help you understand the real differences between each type, what daily life is like with each, and how to decide which approach fits your goals, bite, and budget. Ultimately, it’s here to help you know which is the best denture choice for you.
Quick Pros & Cons Comparison
Traditional (Tissue-Supported) Dentures
✅ Pros:
Most affordable upfront option
No surgery required
Can look very natural
Quick turnaround
⚠️ Cons:
Less stable, especially on lower jaw
Can require adhesive and frequent relines
May accelerate bone loss over time
Harder to chew tougher foods
Snap-In (Implant-Retained) Dentures
✅ Pros:
Secure, “no-slip” fit
Palate often open — better taste and speech
Easy to remove for cleaning
Lower cost than fixed options
⚠️ Cons:
Some rocking during chewing
Attachments wear out every few years
Slightly less bite force than fixed bridges
Fixed Implant Dentures (All-on-X or Hybrid Bridge)
✅ Pros:
Feels and functions like natural teeth
Maximum bite strength and stability
No movement — ever
Restores facial support and confidence
⚠️ Cons:
Highest initial investment
Requires surgery and planning
Harder to remove if hygiene neglected
Questions to Help You Decide
💬 1. Do you need full dentures on top, bottom, or both?
Top only: Any of the three options can work. The upper arch has strong tissue support, so even traditional dentures often hold well.
Bottom only: Implants are strongly recommended. Lower dentures without implants tend to move — the tissue there simply doesn’t provide suction or stability.
Both arches: Many patients choose snap-ins or fixed implants to restore chewing and confidence on both.
💬 2. Are you looking to save cost or invest long-term?
Tight budget: Traditional dentures are the most affordable starting point.
Balance of value and stability: Snap-ins offer excellent function for their cost.
Long-term comfort and lowest maintenance: Fixed implants are the best investment — fewer adjustments, better longevity, and stronger chewing efficiency.
💬 3. How important are esthetics and facial support?
High-end esthetics: Fixed zirconia dentures deliver the most natural look and facial support.
Moderate esthetics: Snap-ins can look great and are easier to adjust.
Good esthetics on a budget: Traditional dentures still provide a beautiful smile when crafted carefully.
💬 4. Do you clench or grind your teeth?
Frequent clenching/grinding: Fixed implants are strongest and distribute force best.
Light or occasional grinding: Snap-ins can work well, but may need stronger attachment materials.
Traditional dentures: Can flex or break if heavy bite force is present.
💬 5. What’s your jawbone and gum strength like?
Strong bone/tissue: Any option is possible.
Bone loss present: Implants can preserve bone and improve fit.
Severe resorption: Bone grafting or strategic implant placement may be advised first.
💬 6. Do you already have dental implants?
Existing implants: You may be able to retrofit a new snap-in denture to them.
No implants yet: Starting with a plan that allows future upgrades (from snap-in to fixed) gives flexibility and control over timing and cost.
Putting It All Together
GoalBest FitLowest initial costTraditional dentureBetter chewing without full surgerySnap-in dentureMaximum stability & estheticsFixed implant dentureUnsure where to startBegin with snap-ins, upgrade later
No two mouths are alike — that’s why every plan we make at Teuscher Legacy Dental starts with imaging, bite evaluation, and a detailed conversation about what matters most to you.
Next Step: Get Clarity Before You Commit
Not sure which way to go?
That’s exactly what our no-charge clarity call is for.
In 10 minutes, we’ll help you understand what fits your bone, bite, and budget — before you spend a dollar.
📍 Serving St. Charles, Campton Hills, Geneva, and Elburn, IL
📞 Call or text (630) 762-0000
💬 Schedule online!
Citations
Feine JS et al. The McGill Consensus Statement on Overdentures. J Prosthet Dent. 2002;88(5):354-358. PubMed PMID: 12447223
Sadowsky SJ. Mandibular Implant-Retained Overdentures: A Literature Review. J Prosthet Dent. 2001;86(5):468-473.
How to Care for Your Dental Implant (and Protect It for Life)
A dental implant is one of the most durable and life-changing treatments in modern dentistry. When done right, it can look, feel, and function like a natural tooth for decades.
But long-term success doesn’t happen automatically — it’s built through partnership.
You take care of it at home.
We monitor, adjust, and protect it in the office.
Together, we keep your implant strong for life.
💡 Your Implant Isn’t Just Metal — It’s a Living Connection
Your implant is a precision-engineered system:
A titanium root fused directly to your jawbone (osseointegration)
A custom abutment connecting that implant to your crown
A crown designed for perfect bite and esthetics
At Teuscher Legacy Dental, we use the best possible implant systems like BioHorizons implants, because small details — implant design, abutment fit, and crown material — make a major difference.
Even a slight bite imbalance (we’re talking microns) can create disproportionate stress on the bone or screw, and lead to implant failure.
That’s why we manage the surgical precision, digital customization, and occlusion balance.
Your role is what this article is about — the daily home care that keeps the gum and bone around your implant healthy.
🪥 Daily Home Care: Gentle, Consistent, and Targeted
1️⃣ Use the Right Tools — Not Just Floss
Traditional floss can fray or cut around implants. It’s generally rougher on the delicate tissues around the implant. Instead, it’s better to use:
Soft-Picks (GUM / TePe Soft Brushes) — flexible silicone tips that sweep gently under the gumline.
ProxaBrushes (interdental brushes) — soft, cone-shaped brushes that fit between implants and neighboring teeth.
Implant crowns naturally create a slightly larger “triangle” space where they emerge from the gum. That’s normal — it’s simply the anatomy of an implant. But that small gap can trap food, so daily gentle cleaning here prevents odor, inflammation, and bone loss.
2️⃣ Brush Twice Daily with a Soft or Electric Brush
Angle bristles toward the gumline and use gentle circular motions. Avoid whitening pastes with heavy abrasives. The Best time, if you could only brush once, is right before bed!
3️⃣ Rinse Wisely
An alcohol-free antimicrobial rinse such as CloSYS or PerioScience AO Gel can help reduce biofilm and inflammation.
⚠️ A word of caution on mouth rinses:
Recent research (and experts like Dr. Andrew Huberman) suggest that routine use of strong antimicrobial mouth rinses may disrupt the beneficial oral microbiome that protects long-term gum and cardiovascular health.
So if you use a rinse, treat it as a tool, not a habit — short-term use during healing or inflammation is fine, but your daily defense should be mechanical cleaning: brushing and interdental care.
At Teuscher Legacy Dental, we’ll guide you personally on whether an antimicrobial rinse fits your situation.
🧠 Professional Hygiene Visits: Modern Care for Modern Implants
Every 6 months — or more often for patients with a history of gum disease or other special considerations — your implant should be cleaned with specialized techniques.
✅ Glycine Air Polishing — The Gold Standard (and the One We Use)
There’s one universally accepted, implant-safe method for cleaning titanium: glycine air polishing. Glycine air-polishing has been shown in peer reviewed studies to effectively remove biofilm from titanium without damaging implant surfaces — a clear advantage over traditional scalers
(Renvertetal.,2015), (Jietal.,2014)
Glycine powder particles are a fraction of the size of traditional polishing paste, making it gentle enough for both the implant surface and soft tissue while still removing harmful biofilm.
At Teuscher Legacy Dental, every implant maintenance visit includes glycine air polishing — the safest, most effective way to protect your implant’s surface integrity and prevent peri-implant inflammation.
Most general dental offices still use metal scalers or standard polish on implants — which can microscopically scratch the surface and invite bacterial buildup. We don’t. Every implant patient at Teuscher Legacy Dental receives true implant-safe maintenance.
⚖️ Why Bite Balance Still Matters (and We Handle That Part)
Because implants don’t have a ligament like natural teeth, they can’t flex or cushion forces. Even a subtle bite imbalance can multiply pressure into the bone or screw.
That’s why:
We use premium implants for precision fit
We design custom abutments to shape soft tissue ideally
We select crown materials that distribute force evenly
We continually monitor your occlusion to keep forces balanced
Those are our responsibilities. Yours is consistency — daily care and keeping your maintenance visits.
⚠️ Gum Disease & Peri-Implant Disease: Know the Risks
Implants can’t get cavities, but the surrounding gums and bone can still get infected:
Gum disease (periodontitis) can spread to implant sites
Peri-implant mucositis = early inflammation (redness, bleeding)
Peri-implantitis = deeper bone loss that threatens the implant
These diseases often start silently — but they’re completely preventable through glycine maintenance and proper home care.
🛠️ Long-Term Protection Tips
Wear a nightguard if you clench or grind.
Stay nutritionally strong — vitamin D, omega-3s, and calcium all support bone health.
Keep your recall visits — X-rays and probing track bone stability early.
Call us early for any bleeding, odor, or looseness — small issues are easy to fix when caught early.
🧾 Common Questions We Hear
Can I polish my implant like a regular tooth?
At home, yes — with a soft brush. In-office, only glycine air polishing should ever touch an implant.
Why does food get caught near my implant?
The “triangle” space is normal anatomy. Use a Soft-Pick or ProxaBrush daily to keep it clear.
Can gum disease come back around implants?
Yes — bacteria don’t care if it’s enamel or titanium. That’s why maintenance is essential.
How long will my implant last?
With balanced occlusion, glycine maintenance, and daily home care, most implants last 25 years or more — often for life.
🏁 The Bottom Line
You’ve invested in something built to last.
We handle the surgical precision, occlusion, and maintenance technology.
You handle the daily care.
Brush gently, clean between teeth, and trust that every recall visit at Teuscher Legacy Dental uses the safest, most advanced methods available.
That’s how we protect your implant — and your confidence — for life.
Teuscher Legacy Dental — Choose Excellence
📍 St. Charles • Campton Hills • Kane County
📧 info@teuscherdental.com | ☎ 630-762-0000
Real Case: Immediate Load Implant Dentures! What Went Wrong (and How We Fixed It)
A Before and After of Mrs. Jones’ full mouth implant denture case at Teuscher Legacy Dental! See what went wrong, and how we fixed it. The entire case is in detail below!
A real, top and bottom full-arch implant denture case from St. Charles, IL
Patient: Mrs. Jones (not her real name)
Clinician: Teuscher Legacy Dental
Surgeon: Midwest Dental Implantology (our surgical partner)
Prosthetic system:
Temporary dentures: Acrylic
Bite and smile adjusted dentures: 3D Printed PMMA with custom glaze
Final dentures: Full-contour zirconia with titanium reinforcement (Rosen technique)
Dr Brayden Teuscher breaks down this immediate load implant denture case in detail!
The Situation: A Patient Frustrated that One Tooth After Another Kept Breaking
Full Face Smile - Before
Retracted view of all teeth - Before
Close up of smile - Before
Mrs. Jones has been a patient of ours in St Charles for years, but kept having one tooth after another break down and need dental work. She is a lovely lady, but frustrated with one tooth problem after another. Her whole life, her teeth had caused her trouble. It’s a situation we hear often! We discussed addressing her smile and bite in one fell swoop - the last restorative dentistry she’d ever need. We discussed some options, and showed her other real cases. In the end, she decided to go with a fresh slate: Full mouth extractions and implants. But she did not want to be without teeth to chew and smile.
The Goal: A Beautiful, Confident Smile - Now. Not Months From Now
Mrs. Jones needed full-arch extractions and immediate implants on both her upper and lower arches. The goal: leave the surgery with teeth to chew and smile with right away away (called immediate load), then refine fit, bite, and esthetics as the tissues heal. Ultimately finishing with a beautiful smile and comfortable bite. In this case “immediate loading” meant 24 hours after implant surgery was completed.
We coordinated with Midwest Dental Implantology for the surgery, and Ottawa Dental Lab for the dentures. This meant a lot of communication with the surgeon and lab on the front end, so that everything would run smoothly for Mrs Jones.
Key idea: With immediate loading, the first prosthesis gets you smiling and chewing right away. The final prosthesis is delivered after healing—when your bite and tissue positions are stable.
Bonus: More info on Implant Supported Denture types and comparison with traditional dentures!
What Went Exactly as Planned
The surgery itself. The teeth were extracted and implants placed. See the panoramic image below.
The new dentures fit perfectly onto the implants. A snug, perfect fit helps control and guide the healing process.
The shade and smile architecture of the new teeth. Mrs Jones was pleased with her new smile right away, and we all knew we may be able to improve it further in the final dentures.
We knew we’d have to make some adjustments to the denture bite! That is always the case with immediate dentures.
What Went “Wrong” (And Why That’s Normal)
Day-after delivery (first acrylic):
Smile looked great! Bruising present from surgery the previous day
Surgery went smoothly. All implants placed.
Immediate bite was slightly open in front and right sides!
Though the smile was great, Mrs. Jones’ right side bite was open. This meant, if she kept those denture teeth, she could not chew efficiently on that side during her healing process. We took a new scan immediately, and Ottawa Dental Lab remade the dentures for next-day delivery. She wore the existing ones home, and the next day we gave her an almost identical pair, with minor tweaks to make the bite just right.
Why did the open bite happen?
The day of surgery, the precise location of the dental implants was captured using Photogrammetry. Patients often assume that because implant dentistry now uses photogrammetry and digital scans, the bite should be “locked in” on day one with zero adjustments. The truth is: photogrammetry captures the precision of the implant positions, but not the biology of the soft tissues and muscles surrounding them.
| Reason | Simple Explanation |
|---|---|
| Swelling | Your gums and cheeks are puffy after surgery, so the bite does not close the same way yet. |
| Muscle Tension | Your jaw muscles are “protecting” the area, so you may not bite fully on one side. |
| New Bite Position | Your brain is learning a new bite, so it needs time to settle and feel natural. |
| Both Arches Done | With no “old” bite to guide it, small changes become noticeable as swelling changes. |
But shouldnt digital dentistry, with all the pre-planning be perfect?
| Concept | What It Really Means |
|---|---|
| Photogrammetry = Accuracy | The scan shows the exact implant positions, not swelling or muscle changes. |
| Healing = Change | Your body is shifting and relaxing during the first few days and weeks. |
| Not a “Mistake” | It’s normal for the bite to be adjusted once swelling goes down. |
Second day (second acrylic denture):
Bite was corrected and comfortable—she wore this during the 6-month healing phase. I did not have a good photo of this one. But the open bite was corrected, esthetics remained the same, and Mrs Jones was comfortable as she healed from the surgery. This temporary denture is very important for a couple reasons:
It allows full smile and comfortable chewing while the tissues heal
It test drives the esthetics of the new teeth and bite. In Mrs. Jones’ case, there were a few things we wanted to improve!
6 months later (After full healing):
We prepare the final smile. To do that right, we:
Raised the vertical dimension (slightly opening the bite) for facial support, youthful esthetics, and tooth display
3D-printed try-in dentures to test the new bite and smile design
New smile and bite filled cheeks better for more youthful facial appearance!
Close up of new smile teeth. They seemed bright.
Close up comparing standard shade B1 to teeth. These teeth are too bright for Mrs Jones!
Try-in issue:
The 3D-printed set was too bright—visibly brighter than a B1 shade tab. Mrs. Jones wanted a light shade than before, but both she and our clinical team agreed it crossed into the “too bright/unnatural” zone.
Our fix:
We custom glazed the 3D printed set to tone brightness and add natural characterization (micro-texture, slight incisal translucency, warmth at the necks). See how it compares to the B1 shade tab below in the before and after photos. She test-drove this new bite and esthetic for a few weeks. It felt right, looked right, and photographed beautifully for her at home.
Before Same-Day custom stain and glaze
After same-day custom stain and glaze to make shade slightly darker
Retracted view of full smile after same-day stain and glaze. This is much more natural looking in a temporary denture!
Bonus: Teuscher Legacy Dental was named “Best Cosmetic Dentist in St Charles, IL in 2025”. We do this type of cosmetic adjustment all the time, and win awards for it!
Final Denture:
We duplicated that approved design in full-contour zirconia with titanium reinforcement (Rosen technique) and delivered the definitive prostheses.
The Result:
Mrs. Jones was thrilled!
A Perfect, Beautiful Bite
Esthetic Zirconia Final Implant Dentures for the top and bottom
“Absolutely perfect.”
Mrs. Jones was thrilled. We called her to follow up a couple weeks after final delivery, and she told us she forgets she ever had it done. Her smile feels as natural as when she was in her 20’s!
Reminder: Why Immediate Load Can Need Tweaks
Post-op swelling shifts the bite (especially in the first 24–72 hours).
Soft tissue and muscle tone change through the healing period.
Implant occlusion (bite forces over the implants) needs precision to protect the implants long-term.
Shade perception changes in different lighting and with lip posture once swelling settles.
This is not failure—it’s quality control. The right approach is: diagnose early → correct promptly → prove the final design with a real-world test. It’s part of why implant supported dentures are more expensive than tissue supported at Teuscher Legacy Dental. We don’t nickel and dime you for every little thing. There is one fee for us to get the job done correctly. Always transparency, nothing hidden!
Why We Increased Her Vertical Dimension (VDO)
Patients ask: “Why change my bite height if the temporary was ‘fine’?”
Because the final smile should support the lips, soften lines, and show the right amount of teeth—without overloading the implants. See more in the table below.
Why We Increased the Vertical Dimension (VDO)
| Benefit | What the Patient Notices | Clinical Rationale (Simple) |
|---|---|---|
| Smoother lines around the mouth | Less folding or “collapse” of the corners of the lips | More facial support from the restored bite height |
| Fuller, more youthful smile | Teeth show properly when smiling and at rest | Proper incisal display improves facial proportions |
| Balanced chewing | Bite feels more even and stable | Vertical dimension protects implants from overload |
| Clearer speech | “S,” “F,” and “V” sounds feel natural again | Tooth position and speaking space improve with correct VDO |
| Better long-term durability | Final teeth feel stable and built to last | Balanced forces reduce wear and implant stress |
Notes for clinicians reading: Classic prosth literature supports evaluating/restoring VDO for esthetics, phonetics, and function (e.g., Turner & Missirlian 1984; Silverman 1956; Abduo & Lyons 2012), with implant texts emphasizing load management and occlusion for longevity.
Material Matters: Provisional vs. Final
Materials Used at Each Stage (and Why)
| Stage | Material | Why We Use It | What Patients Should Expect |
|---|---|---|---|
| Immediate + Healing | Acrylic (chairside/lab) | Fast, repairable, and easy to adjust while tissues stabilize | Looks great day one; expect bite checks/adjustments; not the final set |
| Design Trial | 3D-Printed (Try-In) | Lets us test your new vertical, tooth position, and smile shape | May look “too perfect/bright” before glazing; used for short-term test |
| Approved Design | 3D-Printed + Custom Glazing | Adds natural color, depth, and surface texture before finalizing | Worn for a few weeks → confirm comfort, speech, and appearance |
| Final | Full-Contour Zirconia with Titanium Reinforcement (Rosen Technique) | Strong, highly esthetic, and built for long-term durability | Natural, lifelike, and long-lasting; maintenance preserves your investment |
The Real Workflow (Transparent Timeline)
The Full-Arch Implant Denture Timeline (What Happened and When)
| Step | What Happens | When |
|---|---|---|
| Surgery & Photogrammetry Scan | Full Mouth Extractions + implants placed at Midwest Dental Implantology; Photogrammetry scan that same day | Day 0 |
| Immediate Delivery | Acrylic, implant dentures delivered top and bottom; patient leaves with a full smile. Problem: Open bite on Mrs Jones' right side | Day 1 |
| Early Correction | When bite is off, we rescanned and remade promptly | Day 1-2 |
| Healing Phase | Bite and tissues settle; small adjustments made for comfort; implants fully stabilize | ~6 months |
| Optional Smile Redesign | In this case, We opened the vertical dimension and tested the new smile architecture with 3D-printed implant dentures that the patient wore for a while to test out | After full healing phase |
| Optional Esthetic Refinement | Custom glazing added more natural color, texture, and realism. The initial 3D printed dentures were too bright. | Same day as smile redesign delivery |
| Test-Drive new smile and bite | Patient wears the new dentures and smile in real life — talking, chewing, photos, etc. to make sure it is PERFECT before we deliver the final dentures. | Two weeks |
| Final Delivery | We duplicate the approved design in beautiful Zirconia (Rosen technique) | Final Delivery Day 🎉 about 7 months after surgery in this case |
What Patients Should Learn From This
Immediate load is amazing — you don’t go without teeth.
The first set of dentures isn’t usually permanent, and usually requires adjusting— healing changes things; refinement is normal.
Ultra-white isn’t always “right” — the best smiles add warmth, texture, and translucency. The 3D printed dentures in this case were too bright, but we adjusted them simply to add life and color to Mrs Jones’ smile.
Testing the design in real life (weeks, not minutes) ensures your final looks and feels right. You’re making a big investment! You should feel GREAT about the result.
Team-based care matters — surgery and prosthetics working in sync is how you get predictably great results.
FAQ’s about fixed implant supported dentures
Is it normal to need multiple prostheses?
Yes. You’ll leave surgery with teeth, but the final comes after healing. We adjust design, bite, and esthetics based on real-world wear.
Why not just pick the whitest shade?
Ultra-bright can look flat and fake—especially under daylight and in photos. Characterization (glaze, micro-texture, incisal translucency) makes a smile believable.
Will increasing my bite feel weird?
For a few days, sometimes. That’s why we test-drive your new vertical and smile design before committing to the final.
How long does this take?
Immediate smile: day 1. Healing: about 6 months. Design/test: a few weeks. Final delivery follows promptly after approval.
Partner Acknowledgment
Surgery performed by Midwest Dental Implantology. Lab support from Ottawa Dental Lab. We value collaborative, team-based implant care for safer surgery and better long-term prosthetic outcomes.
Citations
Classic prosthodontic literature ties vertical dimension to facial support, phonetics, and esthetics; implant prosthetics texts emphasize load management and occlusion for longevity (e.g., Turner & Missirlian, J Prosthet Dent 1984; Silverman 1956; Abduo & Lyons, Aust Dent J 2012; Misch, Contemporary Implant Dentistry; Goodacre 2018 review). Translation? The “little” details matter a lot when you want a result that looks natural and lasts.
Ready to Explore Your Options?
If you’re considering full-arch implants in St. Charles, Campton Hills, Elburn, Geneva, or greater Kane County, we’re happy to walk you through immediate load, the test-drive process, and final zirconia options—and show you examples like Mrs. Jones.
-Dr Brayden Teuscher
How Soon After an Extraction Can I Get a Dental Implant?
If you’ve been told a tooth needs to come out, your next question is probably:
“How soon can I get an implant?”
That’s a smart question — timing matters more than most people realize. The short answer: in some cases, immediately (the same day as your extraction). In others, it can take several months before your bone is ready. Here’s how to know what’s best for you.
🧠 The Science Behind Timing
After a tooth is removed, your body starts remodeling the bone that used to hold it. Within 3–6 months, up to 40–60% of the ridge width can shrink if left untreated (Araujo & Lindhe, J Clin Periodontol, 2005). Once that bone is lost, replacing it becomes more complex — less predictable and more expensive. Usually it requires “lateral ridge augmentation” -a topic for another blog post.
So at Teuscher Legacy Dental, before getting a tooth out, we always plan tooth replacement with the end in mind — preserving bone from day one so your future implant has a strong, stable foundation.
⏱️ The Three Most Common Implant Timelines
1. Immediate Placement (Same Day as Extraction)
Immediate placement means the tooth is pulled and the implant screw goes in the same day. We detailed one of our own immediate implant cases here.
When it works best:
The bone around your tooth is intact
There’s no infection
You want to preserve gum and bone shape
Most often possible in single root teeth (less likely for molar teeth)
Why it matters:
Immediate implants reduce overall treatment time and minimize bone loss. It’s the gold standard when conditions allow — but it requires precise surgical skill and 3D imaging to ensure stability.
2. Early Placement (6-12 Weeks After Extraction)
When it works best:
Minor infection or bone irregularities were present
The site needs short healing before implant stability
Specific bone grafting protocols are used to allow quicker bone healing
Why it matters:
This approach lets the gum tissue heal and keeps the bone active enough to avoid major resorption. If you get a bone graft, using the right type of bone graft is hugely important, and it must integrate well with the implant system being used. See the table below for more information.
Types of Bone Grafts and Healing Timeframes
| Bone Graft Type | What’s In It | When It’s Used | Typical Healing Timeframe |
|---|---|---|---|
|
Collagen-Based Synthetic Graft (OsteoGen Plug) |
Collagen matrix combined with bioactive calcium phosphate that resorbs as natural bone fills in. |
Used for 4-walled extraction sockets or sites with minimal infection. Ideal when socket walls are intact and a membrane is not required. |
4–6 months for bone to fully mature before implant placement. |
|
30/70 Cortical–Cancellous Mix |
30% cortical (dense) bone and 70% cancellous (spongy) bone particles, often covered with a collagen plug or membrane. |
Used for 3- or 4-walled extraction sockets that need faster healing with good volume maintenance. |
8–12 weeks before implant placement or soft-tissue coverage procedures. |
|
70/30 Cortical–Cancellous Mix |
Higher ratio of dense cortical bone for slower resorption and long-term ridge support. Typically used with a resorbable membrane. |
Used for ridge augmentation or sites missing one or more walls, where added structure is needed for future implant stability. |
3–5 months for full maturation before implant placement. |
|
Xenograft (Bovine or Porcine-Derived) |
Deproteinized bone mineral from animal sources; primarily an anorganic hydroxyapatite scaffold that resorbs very slowly. |
Sometimes used for esthetic volume preservation when long-term contour is desired, but not ideal for implant integration. Not used at Teuscher Legacy Dental. |
Can remain for years; offers volume stability but limited new bone turnover. |
3. Delayed Placement (3-6 months after extraction)
When it works best:
Larger bone grafting was done at extraction
Significant infection or bone loss was present prior to extraction
A synthetic bone graft was used
The site needs full regeneration before implant placement
Why it matters:
Sometimes slower is smarter. Allowing the graft to mature ensures the implant integrates with dense, healthy bone for long-term success — even if it takes a few extra months.
After a tooth is pulled, the socket is often filled with a bone graft
The collagen plug and sutures after the bone graft was placed
🧩 Tell Me More About Bone Grafts
If the bone is thin, soft, or missing in key areas, a bone graft can preserve or rebuild it. Think of it like “soil preparation” before planting — it gives the implant a strong, lasting foundation.
In Kane County, socket preservation grafts typically cost between $700 and $900 per site, but they can prevent much larger future surgeries. At Teuscher Legacy Dental, the most common type of bone graft (socket preservation) is $869.
Here’s an example of a REAL extraction and bone graft case from Dr Brayden Teuscher at Teuscher Legacy Dental.
📷 Why Digital Planning Makes All the Difference
At Teuscher Legacy Dental, every implant case is planned with 3D cone beam CT imaging and digitally designed surgical guides — the same technology used by other leading surgical centers.
This allows us to:
Visualize bone quality, and sinus anatomy, and nerve locations
Place implants with extreme precision
Often shorten healing time and improve comfort
Optimize location of future crown (the chewing part of the implant)
(Source: Vercruyssen et al., Clin Oral Implants Res 2014;25:94–99)
❤️ What Patients Love About This Approach
Our patients tell us they appreciate:
Clear timelines before surgery
Clear communication about all risks involved. Our reviews often mention how we take the time to listen to our patients’ questions and fully explain everything when they need!
Gentle extractions that protect surrounding bone
Predictable healing with high quality bone grafting and implant techniques
Transparent pricing (no surprise fees). We go over all fees before we ever take the tooth out, and there are no hidden fees. If other offices aren’t transparent about their pricing, check our implant pricing guide and tips resource.
📅 Bottom Line
The right timing for your implant depends on:
The health of your bone and gums
Whether infection or bone loss is present
If a graft or membrane was used, and what type
Your overall healing and goals
At Teuscher Legacy Dental, we’ll evaluate your 3D scan and tell you — clearly and honestly — what’s possible now and what may need a few months of healing first.
Frequently Asked Questions
Can I get a dental implant the same day my tooth is extracted?Yes, in some cases. Immediate implant placement works best when the surrounding bone is strong, there’s no infection, and the tooth is a single-rooted tooth. It helps preserve gum and bone shape and shortens total treatment time. |
How long should I wait after an extraction before getting an implant?Most patients can safely have an implant placed between 8–12 weeks after extraction if early bone healing is complete. For sites that had infection or bone grafting, the healing period may extend to 3–6 months. |
Do I always need a bone graft before getting an implant?Not always. If the bone walls are intact and thick enough, a graft may not be necessary. But when infection, bone loss, or thin socket walls are present, a graft protects the ridge and prevents future bone collapse. |
How much does a bone graft cost in Kane County, IL?Socket preservation bone grafts in our area typically range between $700 and $900 per site. At Teuscher Legacy Dental, the standard grafting fee is $869, and all costs are reviewed before any procedure begins. |
Does digital planning really improve implant results?Yes. 3D CBCT imaging and guided surgery technology allow us to visualize bone density, nerve pathways, and implant angulation before placement — leading to more predictable healing, faster recovery, and ideal aesthetics. |
What happens if I wait too long after an extraction?Bone naturally resorbs after a tooth is removed — up to 40–60% of ridge width in 3–6 months. Waiting too long can require more complex bone grafting later or make implant placement less predictable. |
What are the Next Steps?
If you’ve had an extraction (or know one is coming), schedule a Free Implant Consultation today. We’ll review your imaging, discuss your options, and create a timeline tailored to your mouth and goals.
👉 Schedule Online or call (630) 762-0000
-Dr Brayden Teuscher
Do I Need a Bone Graft After a Tooth Extraction?
If you’ve been told you need a tooth pulled, you might also hear your dentist mention a ‘bone graft.’ What does that really mean—and do you actually need one? This post gives research backed answers to those questions!
If you’ve been told you need a tooth pulled, you might also hear your dentist mention a ‘bone graft.’ What does that really mean—and do you actually need one?
🩺 What a Bone Graft Does (in plain English)
The “socket” is the hole left over after the tooth is extacted.
When a tooth is pulled, there is a hole in your mouth! This is called the tooth socket.
If nothing is done at this point, your body heals by flowing blood into the socket and clotting, forming a “scab”. Eventually
(over about 3 months), this “scab” turns into natural bone and gum tissue. The hole is only there for about 2 weeks, because the gums heal faster than the bone.
Here’s the risk of not grafting: As the bone heals, it collapses from the cheek side.
When the bone and gums collapse, it causes a sunken-in appearance in your bone and gum tissue. Here’s when that bone collapse can be a problem:
If the collapse is in your smile line, it can be unaesthetic
If the collapse is where a future implant may be placed, often the collapse will mean there isn’t enough bone to predictably place an implant. This is the bigger concern usually with bone grafting.
This collapse happens fast. See the table below for multiple studies showing the same thing. In basic English: 8-12 weeks after the tooth was pulled, over HALF of the bone tends to be lost without bone grafting.
| Source (Full Citation) | Timeline Studied | Avg. Horizontal Bone Loss | Avg. Vertical Bone Loss | Key Takeaway |
|---|---|---|---|---|
| Araujo, M. G., & Lindhe, J. (2005). “Dimensional ridge alterations following tooth extraction: An experimental study in the dog.” Journal of Clinical Periodontology, 32(2), 212–218. | 8 weeks | ≈ 50% loss | — | Majority of ridge reduction occurs in the first 2 months. |
| Schropp, L., Wenzel, A., Kostopoulos, L., & Karring, T. (2003). “Bone healing and soft tissue contour changes following single-tooth extraction: A 12-month prospective study.” International Journal of Periodontics & Restorative Dentistry, 23(4), 313–323. | 12 months | ≈ 50% (~5–7 mm) | 1–2 mm | Two-thirds of shrinkage occurs within 3 months. |
| Tan, W. L., Wong, T. L., Wong, M. C., & Lang, N. P. (2012). “A systematic review of post-extraction alveolar ridge dimensional changes in humans.” Clinical Oral Implants Research, 23(Suppl 5), 1–21. | 6 months | 3.8 mm (mean) | 1.24 mm (mean) | Most bone loss happens early and is irreversible without grafting. |
| Van der Weijden, F., Dell’Acqua, F., & Slot, D. E. (2009). “Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review.” Journal of Clinical Periodontology, 36(12), 1048–1058. | 3–6 months | 29–63 % | 11–22 % | Majority of loss occurs in the first 3–6 months. |
| Misch, C. E. (2015). Contemporary Implant Dentistry (4th ed.). St. Louis, MO: Elsevier Mosby. | 6 months (summary) | Up to 60 % | Up to 40 % | Grafting at extraction maintains ridge form and simplifies future implant placement. |
Why does the bone loss matter?
It makes placing an implant less predictable, because implants need enough bone to support them long term.
What if I decide I want an implant later, but the bone has already collapsed?
In this case, different types of bone grafting are available. But it is usually more expensive and less predictable than filling the original tooth socket would have been.
When a Bone Graft Is Usually Recommended at the time of Tooth Extraction
You plan to get a dental implant in the future
Front tooth (esthetic zone) where gum shape matters
Larger infection or cyst that has already removed a large portion bone
Thinner bone around roots
In our St. Charles practice, roughly 6 out of 10 extractions include socket preservation because it prevents risk of a bigger surgery later.
⚖️ When A Bone Graft Might Be Optional (or you may not want one)
Molar tooth with no plan for implant
Already has thick bone support
Significant infection where graft won’t integrate well initially
Cost is a reason people choose against a bone graft
Ultimately, the best decision depends on your long-term plan for that space—if you want an implant, grafting right away usually saves you both time and money later. It also keeps options open should you change your mind about an implant later. If you definitely dont an implant, the graft is usually less important.
💰 Cost in the Kane County, IL Area
Range: $700–$1,000 per tooth in Kane County
Insurance typically covers part if related to tooth loss
At Teuscher Legacy Dental, our fee for a socket preservation graft is $936. That fee includes appropriate healing membrane, sutures, and follow ups as necessary.
Watch out- often you may be quoted a lower fee for a bone graft, but additional fees for a healing membrane and other peripherals. Don’t get taken advantage of! For more tips on how to price compare this type of procedure, check our implant pricing blog post.
📸 Section 5: Real Case Example (Before/After Photos)
Here’s a case where Dr Brayden Teuscher extracted a molar tooth and placed a bone graft. We detailed this case further in this blog post. And, you can see how this case progressed and we planned and placed the implant here.
X Ray of Molar Before Extraction
Photo of Molar Before Extraction
Photo of Tooth Socket After Extraction, Before Bone Graft
X Ray of Extraction Socket, after filling with bone graft
Photo of bone graft with collagen plug and white sutures over the top
🙌 What to Expect During Recovery
Some pain, bleeding, and swelling are normal! Usually at Teuscher Legacy Dental we see you for a post operative check and suture removal at 1 week after the procedure. Below I pasted the words from our post operative instructions that we give to every patient after this type of procedure:
1. Bleeding
· Keep the gauze in place, biting down firmly for 30-45 minutes.
· If bleeding persists, use wet gauze and bite down for another 30 minutes. Always wet gauze before placing or removing it. A damp black tea bag can also be used for this purpose
· Oozing for up to 48 hours, especially at night, is normal.
2. Managing Sensitivity and Swelling
· Take any recommended medication as directed.
· Apply an ice pack near the extraction site for 15 minutes on, 15 minutes off during the first 24 hours.
· Switch to a warm compress after 48 hours to improve healing.
· Sensitivity may be more noticeable at night—sleeping with your head elevated may help
3. Avoid Disrupting the Clot
· Avoid rinsing, spitting, or using a straw for 24 hours.
· Do not smoke or vape for at least 48-72 hours—this increases the risk of dry socket.
· Stick to soft, cool foods; avoid anything hot, crunchy, or spicy. Also avoid foods that may get lodged in the socket
4. Bone Graft Care
· If a bone graft was placed, do not touch or disturb the area, including the stitches or membrane if placed.
· It is normal for small granules or particles to leak out during the first few days.
5. Oral Hygiene
· Brush and floss normally, avoiding the extraction site for 24 hours.
· After 24 hours, you can rinse gently with warm saltwater (1/2 teaspoon salt in 8 oz water) 2-3 times daily.
o If you choose to do this, be gentle. If it is irritating, stop.
6. Rest and Recovery
Limit physical activity for the first 24-48 hours. Rest with your head slightly elevated to minimize swelling and bleeding
7. Contact us IF:
· Excessive bleeding that does not stop after applying pressure for 1-2 hours.
Signs of infection, such as fever, chills, severe pain, swelling, or foul-tasting drainage from the extraction site.
Numbness or tingling that persists for more than 24 hours.
If one of the above occurs and you are unable to reach us, go to the nearest hospital Emergency Room.
🧠 FAQ’s
Frequently Asked Questions About Bone Grafting After Tooth Extraction
| Question | Answer |
|---|---|
| How long does a bone graft take to heal? | Most socket grafts heal in 3–6 months before an implant can be placed. Factors like overall health, graft material, and site location can affect healing time. Learn more in our post on bone graft preservation case . |
| Can you get a dental implant without a bone graft? | Yes — but only if there’s enough bone remaining to stabilize the implant. In many cases, skipping grafting after extraction causes significant bone loss within months, as discussed in our dental implants guide . |
| Is bone grafting painful? | No — with modern techniques and gentle care, most patients describe it as mild soreness similar to an extraction site. Our team uses advanced methods discussed in our St. Charles tooth extraction page to keep you comfortable during recovery. |
| What happens if I skip bone grafting? | Without a graft, the socket shrinks rapidly—losing up to half its width in just a few months. That can make future implants or bridges more difficult and expensive. See the full breakdown of costs and timing in our dental implant pricing article . |
| What materials are used for bone grafting? | We use biocompatible materials such as allograft (human donor bone), xenograft (bovine), and synthetic grafts, often covered with a collagen membrane and PRF to enhance healing. Details and case examples are shown in our bone graft case study . |
Information in this article is based on studies published in the Journal of Clinical Periodontology, International Journal of Periodontics & Restorative Dentistry, and Clinical Oral Implants Research. Clinical examples and post-operative guidelines are from Teuscher Legacy Dental’s own St. Charles, IL practice.
More Resources!
🧭 Want to Consult in Person? Or Want us to pull your tooth?
If you’re facing an extraction, our trained, award winning team in St. Charles can help you understand whether bone grafting makes sense for you—and show real examples of how it preserves your smile for years to come.
Schedule your visit →
My Tooth Hurts — Does It Need to Be Extracted? How to Know What’s Next
By Dr. Brayden Teuscher, Teuscher Legacy Dental — St. Charles, IL
💬 The Real Question People Ask
“My tooth’s been hurting on and off. Does that mean it needs to be extracted? — or could a filling or crown still save it?”
That’s one of the most common (and stressful) questions we hear.
No one wants to lose a tooth — and the truth is, extraction should always be the last resort, not the first option.
At Teuscher Legacy Dental, our job is to find out why it hurts before deciding what to do.
🔎 Step 1: Understand What the Pain Means
Tooth pain doesn’t always equal extraction.
Here’s how different types of pain often point to different causes:
| Type of pain | What it might mean | Typical solution |
|---|---|---|
| Sharp pain when chewing | Small crack or high bite | Bite adjustment or crown |
| Sensitivity to cold | Reversible inflammation | Desensitizing care or minor filling |
| Lingering ache after hot/cold | Nerve infection | Root canal or extraction |
| Throbbing pain or swelling | Abscess or deep infection | Root canal or extraction with graft |
| Dull pressure pain | Sinus pressure or clenching | Bite adjustment or night guard |
🦷 Step 2: Decide — Save or Extract?
We can usually save a tooth if:
The crack doesn’t extend below the gumline
There’s enough healthy structure for a crown
The bone around the root is stable
The root canal system can be properly treated
Extraction is the better choice if:
A vertical root fracture is confirmed on 3D imaging
There’s chronic infection or bone loss around the root tip
The tooth has failed multiple root canals
Mobility makes the tooth unstable
When extraction is necessary, it’s because the long-term prognosis is hopeless — not simply because the tooth “hurts.”
🧭 Step 3: What Happens After Extraction
If a tooth does need to be removed, your next question should be:
“How do I keep the bone from shrinking?”
That’s where socket preservation (bone grafting) comes in.
By placing bone material right after the extraction, we maintain the shape of your jaw so you can easily replace the tooth later — often with a dental implant.
Learn more: ➡️ A Real Patient Example of a Bone Graft After Extraction
⚖️ Step 4: Implant vs Bridge — What’s the Best Replacement?
When it’s time to replace the tooth, you’ll typically have two main choices (but I wrote a full comparison of these dental implant alternatives here):
1. Dental Implant
Replaces the root and the crown
Preserves bone and surrounding teeth
Can last decades with proper care
Doesn’t rely on neighboring teeth for support
2. Dental Bridge
Uses the two adjacent teeth as anchors
Fills the missing space with a porcelain “pontic”
Can be a good option when implants aren’t feasible (for example, if bone volume or medical conditions limit surgery)
However, a bridge requires reshaping the neighboring teeth — even if they’re otherwise healthy — and it does not prevent bone resorption under the missing tooth.
That’s why the American College of Prosthodontists recommends dental implants as the preferred single-tooth replacement whenever conditions allow:
“Implants demonstrate higher long-term survival rates and superior preservation of alveolar bone compared with conventional fixed dental prostheses.”
— American College of Prosthodontists Clinical Practice Guidelines, 2021
Additionally, a systematic review in the Journal of Prosthetic Dentistry found that:
“Single-tooth implants have a 10-year survival rate exceeding 95%, while fixed dental bridges average 80–85%.”
— (Pjetursson et al., J Prosthet Dent 2018;119(2):220–228)
So, while bridges can be appropriate in certain cases, implants typically provide the most stable, natural-feeling, and long-lasting result.
🤝 Step 5: Our Philosophy
If a tooth can be predictably saved, we definitely save it.
If it can’t, we’ll help you decide the best option for you.
Either way, you’ll understand why — before we do anything.
📍 Serving St. Charles, Campton Hills, Geneva & Elburn IL
Teuscher Legacy Dental provides comprehensive surgical and restorative care — from gentle tooth extractions and bone grafts to guided dental implants and smile makeovers — all under one roof. Come see us!
🦷 Real Bone Graft Case: How We Preserve Bone After a Tooth Extraction (Part 1)
By Teuscher Legacy Dental – St. Charles & Campton Hills, IL
When most people think about tooth extractions, they imagine a simple “pull and heal.”
But modern dentistry allows us to preserve the bone where the tooth used to be — usually for setting the stage for a future dental implant that looks and functions like a natural tooth.
This post walks you through a real case from our practice showing what happens before, during, and right after bone grafting. There are different types of bone graft procedures- this one is technically a “socket preservation graft” because it “preserves” the “socket” where the tooth used to be, by filling it with bone. So for this post that’s the type of graft we mean if we say “bone graft”.
In part 1, we will show and discuss the actual extraction and bone graft procedure. In Part 2, we’ll show how it healed and how we planned the dental implant using 3D CBCT imaging.
But First: should you even get a bone graft? Why do you need one? When is it OK to not have one?
I’ll give more detail in a future post. But below is a little more information. The short story is, socket preservation isn’t mandatory for every extraction — but it’s usually the smartest long-term choice if you plan to replace the tooth with an implant.
Here’s how the benefits and risks of socket preservation grafts compare:
| Decision | Benefits | Possible Risks / Costs |
|---|---|---|
| Perform Bone Graft (Socket Preservation) |
|
|
| Skip Bone Graft (No Preservation) |
|
|
Sources: Araujo & Lindhe 2005; Misch 2015; Pikos MA 2019; Kois Center Clinical Protocols.
👀 Step 1: Pre-Op Evaluation
Before removing the tooth, we assessed bone health and root position with detailed imaging. In this case, the tooth had a prior root canal and a cavity on the back side, which caused the crown to loosen and eventually fall off. This tooth could not be saved by a new crown, so it needed to be extracted to prevent risk of infection and further damage of surrounding tissue. After reviewing alternative options, this patient is planning on a future dental implant to restore the site.
Images:
X Ray of tooth #18 Prior to Extraction
Photo of tooth #18 prior to extraction
✅ Purpose: understand root formation, nerve anatomy, and ensure the socket walls are intact for grafting.
🦷 Step 2: Tooth Extraction
After gentle removal, the socket (the bony hole where the roots sat) is clearly visible.
Left alone, this socket starts to shrink immediately — studies show 30–60 % of ridge width can disappear within the first year after extraction (Araujo & Lindhe, Clin Oral Implants Res, 2005). That bone loss often makes future implants more difficult and can even affect facial contours.
Image:
The socket after gentle extraction.
*note for the adjacent tooth - we also did crown #19 that day, and this was before we cemented the temporary crown.
✅ Goal: Gentle extraction maintains socket integrity, keeping bone walls present, and prevents early bone collapse.
🧪 Step 3: Bone Graft and Collagen Plug
To prevent bone collapse, we placed a biocompatible bone graft into the socket.
The material acts as a scaffold that your body gradually replaces with living bone. Usually these bone grafts are from human cadavers, (allograft) but can also be from your own body (autograft), cows or horses (xenograft), or completely synthetic (alloplast).
In our case, we used a cadaver bone particle mix to fill the socket. A collagen plug and PTFE non-resorbable sutures were added to stabilize the area and protect the graft during healing.
Images:
A clear picture of the collagen plug over the top of the bone graft. You can see two of the white sutures as well.
After the bone graft. Notice where the roots used to be, the socket appears filled with bone particulate.
✅ Goal: preserve ridge volume, gum contour, and future implant site quality.
From here, the body takes over — blood flows into the bone graft and forms a clot- eventually forming new bone inside the socket over the next several weeks.
⏱ What’s Next
In Part 2, we’ll show:
The one-week post-op appearance
The 8-week CBCT scan showing regenerated bone
How we plan precise implant placement using guided surgery
💬 Why We Share Cases Like This
We believe you deserve transparency.
Seeing the actual process (not just a before-and-after) helps you understand why bone preservation matters and what is actually happening in the bone graft procedure.
Once bone is lost, it’s more expensive and less predictable to rebuild. Preserving it early gives you more control, fewer surgeries, and a more natural final result.
📍 About Teuscher Legacy Dental
St. Charles & Campton Hills, IL
Family-run, fee-for-service practice specializing in advanced surgical and cosmetic dentistry.
🏆 Voted Best Cosmetic Dentist in St. Charles 2025 by Business Rate.
Learn more about:
🔜 Coming Soon: Part 2
“How Bone Grafts Heal: 8-Week CBCT Results and Implant Planning”
We’ll show real post-op images, bone density changes, and how careful socket preservation makes precise implant placement possible.
Why Choose Teuscher Legacy Dental for Your Dental Implants
The difference between a dental implant and your dental implant is who places it, what materials and implant they use, how well they plan it, the quality of the final restoration, and the experience you have every step of the way.
If you’re considering dental implants in Campton Hills, St. Charles, or anywhere in the Fox Valley region, here’s why choosing Teuscher Legacy Dental is one of the smartest decisions you’ll make. AND- also why Teuscher Legacy Dental may not be the best fit for you! We will always be honest with you.
1. Expert Surgical Skill + Comprehensive Treatment Planning
Training & continuing education
Dr. Brayden Teuscher (and our surgical team) train with the top institutes (Kois, Spear, Implant Pathway, etc.), staying current in implantology, guided surgery, bone graft techniques, and full-arch protocols.Digital 3D planning & guided surgery
We use CBCT imaging and digital surgical guides so your implant is placed with precision, reducing risk and improving outcomes.Top quality implants and other materials
Not all implants are created equally. The brand of implant matters. We exclusively place Biohorizons dental implants, most often Tapered Pro. We also use top of the line bone grafting materials and techniques when necessary. It would be easy to cut costs and use inferior products, but we wont do that. More info on pricing is below!
Full scope of care under one roof
From extraction → grafting → implant → final crown/restoration, we coordinate and complete all phases to minimize surprises and preserve your comfort. One of the main reasons to see Teuscher Legacy Dental instead of a board certified oral surgeon is we can do the required surgeries and restorations all under one roof.High success & low complication mindset
We pride ourselves on strict surgical protocols, sterility standards, and careful case selection to maintain excellent outcomes.
2. Patient Comfort, Transparency, & Trust at the Core
Warm environment + aesthetic facility
From waiting room to surgical suite, we’ve designed a space that calms nerves, not raises them. See our reviews for proof that people from all around the Fox Valley feel relaxed with Teuscher Legacy Dental!Sedation / comfort options available
Oral sedation is available so you feel safe, relaxed, and in control. The TV’s on the ceilings are a digital sedative! And we have blankets, extra pillows, essential oils as needed. Many patients also choose to listen to their own headphones with music or a podcast.No hidden costs & clear financial pathways
We believe in transparency. You’ll see a breakdown of costs, grafting, implants, etc. More detailed cost info for us and any implant provider in St Charles, IL area here. We also offer in-house membership and flexible financing to help you make the investment.Real patients, real stories
Teuscher Legacy Dental showcase REAL before/after cases so you can see the quality and consistency you can expect. They aren’t AI enhanced or models. Other dental offices mostly are using stock photos on their advertising and websites.We’re personable, approachable, and human
You’re not a number. From your first call to follow-up care, you’ll interact with doctors and team members who value your peace of mind. Just look at our reviews for proof!
3. Locally Special, Regionally Trusted
Award-Winning Campton Hills & St. Charles roots
Voted Kane County Chronicle Best of the Fox in 2022 and 2024. Won BusinessRate’s Best Cosmetic Dentist in St Charles, IL in 2025
Serving the entire Fox Valley region
Many patients travel from across Batavia, Geneva, Elburn, and several fly in from out of state, because they know we provide care worth the distance.Competitive but not bargain
We differentiate on value, outcome, comfort, and trust. Our price ranges are slightly above average, generally around 70th percentile in the area.Community reputation + awards
Our cosmetic awards, patient reviews, and community presence strengthen credibility in a competitive market. Check us out on Facebook!
4. Depth of Content & Education Built In
Educational resources tailored to your case
You’ll find in-depth blog posts like “How we restored a front tooth with an immediate implant”, “How Implants Compare to Bridges or Dentures”, “What are the most common implant complications”, and more.Video + visual assets to demystify the process
We use video, animations, and X‑ray case studies so you can see and understand every phase. Check our recent blogs or our YouTube Channel. More on the way!FAQ sections built for your questions
We anticipate what you’ll wonder — pain, recovery, longevity, failure rates — and answer transparently.
5. What Sets Teuscher Legacy Dental Apart
| Differentiator | Why It Matters to You | How Teuscher Legacy Dental Proves It |
|---|---|---|
| A beautiful, calming office and a genuinely welcoming team | Your comfort matters — especially before and during surgery | We designed our space to feel like home, not a hospital. See our tour, team smiles, and real patient reviews. |
| We handle everything in one place — no referrals | Less running around means more consistent care and fewer surprises | From tooth removal to final implant crown, everything is done here by the same trusted team. |
| Aesthetic expertise that goes beyond “functional” | You want your new tooth to look as good as it works | We blend cosmetic precision into every implant — see our smile gallery and natural-looking results. |
| Transparent pricing and flexible financing | No one likes financial guesswork when it comes to their health | We walk you through your cost options clearly — and offer membership and payment plans to help. |
| Approachable, relatable doctors you can trust | Feeling comfortable with your provider is half the experience | Get to know us through intro videos, patient testimonials, and the way people talk about us in reviews. |
⚠️ Break to discuss Why We Might Not Be the Right Fit for Your Dental Implants
At Teuscher Legacy Dental, we’re confident in the care we provide — but we also know we’re not the perfect fit for every implant case. Here are a few situations where we may not be your best option:
1. You're Looking for the Absolute Cheapest Implants
We’re not the most expensive option — but we’re also not a “$999 implant special” clinic. If you’re strictly price-shopping, there are providers in the area that may better suit that goal. For the cheapest possible deal, you’ll be able to find plenty of places that offer “budget implants”. The best way to do that is Google “inexpensive dental implant near me” or something similar. Those offices tend to be running ads and you’ll see them pop up at the top of the search.
Bonus resource below for the deal hunters!
If you are trying to find ways to save money on dental implants, there are several tips and tricks here: Ways to Save on Dental Implants in St Charles, IL
Our dental implant, custom abutment, and crown come in at $6,100 total. We believe we provide excellent value at that price point.
2. You Require Total IV Sedation for Implant Surgery
While we offer oral conscious sedation and many of our dental implant patients have found that to be super helpful, we do not offer IV sedation or general anesthesia in-office. IV sedation or general anesthesia are when you actually “go to sleep” and are unconscious.
If you:
Have dental anxiety that can’t be managed with oral sedatives
Have a strong preference for being fully asleep during any procedure
Have a medical history that makes full sedation the safest route
...then you may be better served by an oral and maxillofacial surgeon (OMFS) with hospital privileges and/or IV sedation capabilities.
In fact, when you need deeper levels of sedation, here are the three oral surgeons near St Charles that we refer to most frequently:
🦷 Dr. Scott J. Genutis, DDS, MS
Campton Square Oral & Maxillofacial Surgery
40W165 Campton Crossings Dr., St. Charles, IL 60175
(630) 513‑6440
(Dr. Genuitis gets a bonus for being Teuscher Legacy Dental’s next door neighbor!)🦷 Dr. Matthew G. McKnight, DDS, MD
McKnight Oral, Maxillofacial & Dental Implant Surgery
605 Courtyard Drive, St. Charles, IL 60174
(630) 377‑7077🦷 Dr. Herbert D. Stith, DDS
Stith Oral & Maxillofacial Surgery
1131 Randall Court, Geneva, IL 60134
(630) 208‑6700
3. You Have Advanced Medical Complexity
We are experienced in handling medically stable patients with common conditions (e.g. controlled diabetes, hypertension, osteoporosis).
However, certain health issues may require care from an OMFS, especially if you have:
Severe immunocompromise
Severe bleeding disorders
Need for general anesthesia due to complex treatment plans
Certain cases with advanced bone loss requiring extensive bone grafting
If your case is outside the scope of safe in-office treatment, we’ll guide you honestly — and help you get care with the right specialist. We will make sure you are safe!
Final Thought: Trust Is Built on Transparency
If we’re not the best choice for your case, we’ll tell you — and we’ll even help you find the provider who is. But if you're looking for a high-trust, high-quality dental implant experience with expert care in a comfortable, patient-first environment… we’d be honored to meet you.
6. What You Should Ask Before Signing Up for Dental Implants
While shopping for an implant provider, here are questions you should consider asking:
Do they perform the entire surgical plan (including grafting) in-house?
What implant brand do they use?
What are possible “hidden fees”?
Do they use guided surgery / digital planning to reduce risk?
What is their success / complication rate?
How do they manage comfort, sedation, and pain control?
What are the refund or re-treatment policies if complications occur?
Do they offer financial flexibility? Under what terms?
Do reviews and testimonials reflect both surgical/restorative skill and patient care?
7. What You Can Expect: The Implant Journey with Us
More information on dental implant timeline here. But here is a brief overview:
Complimentary consult & 3D scan — We assess your bone, plan virtually, and show you treatment options.
Tooth extraction / grafting (if needed) — Conserving bone, placing graft when needed, letting healing take place.
Implant placement (surgery day) — Guided, precise, under comfortable sedation.
Healing & osseointegration — We monitor your progress, adjust, and manage expectations.
Abutment & restoration (crown / bridge / overdenture) — High-quality, esthetic, functional final prosthetic.
Maintenance & follow-up care — Regular checkups, hygiene, and monitoring to protect your investment.
At each stage, you’ll have clarity, choice, and comfort. No surprises.
8. Ready to Start? Here’s Options onHow to Move Forward
Call or text us today at 630-762-0000
Watch our short video case gallery and see transformations
Read related posts on our blog page
Meet Dr. Brayden in his bio section